Article reviewed and approved by Dr. Ibtissama Boukas, physician specializing in family medicine
The term myelopathy means any pathology concerning the spinal cord. Whatever the causes, the myelopathy is a serious illness. It is manifested by various symptoms including paralysis.
This article provides you with details on the different possible locations of the myelopathy, the different causes found, the symptoms, the means of diagnosis and above all the possible treatments.
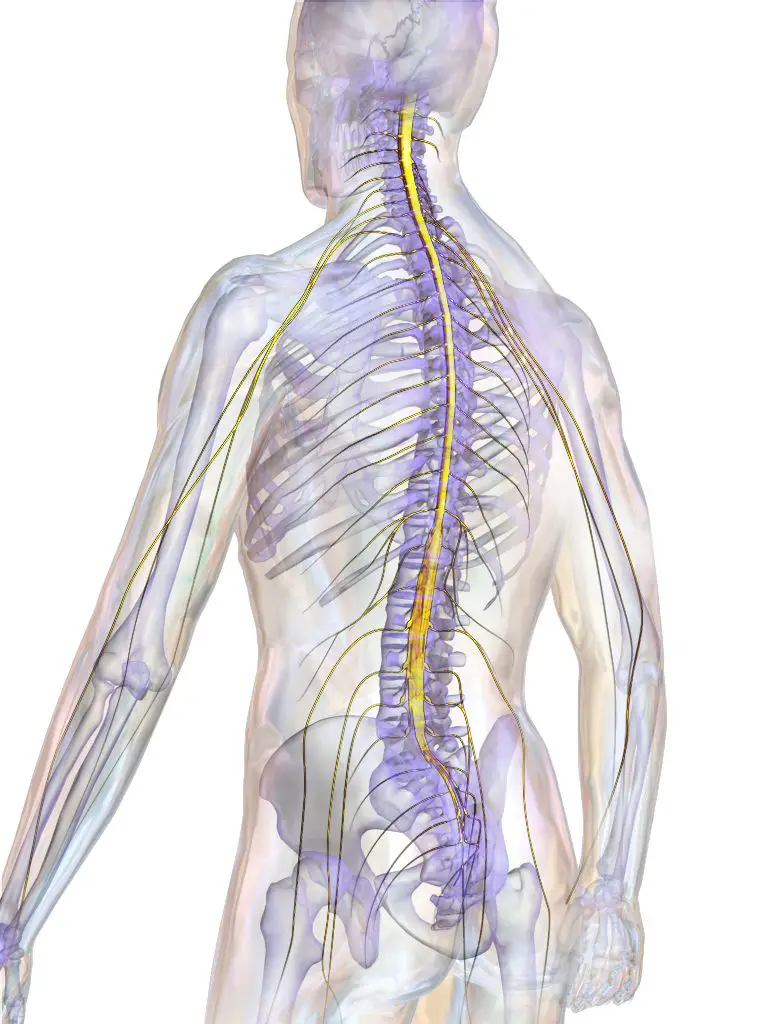
Definition and anatomy
La spinal cord is an organ extending from the neck to the lower back. All its parts can then be affected by the myelopathy. However, the most frequent and the most serious is the cervical myelopathy. Its seriousness lies in the fact that a spinal cord injury at this location will lead to a tetraplegia (paralysis of the four limbs of the body).
La dorsal myelopathy is rarer but also leads to pain in spinal cord. Regarding the lumbar myelopathy, it is associated with the syndrome of narrow lumbar canal. Any narrowing of the dorsal canal can therefore cause compression and pain in the spinal cord (dorsal myelopathy), and in addition, lead to neurological disorders. The dorsal myelopathy is rather rare, compared to narrowing of the lumbar canal and the cervical canal.
Causes of Myelopathy
La myelopathy appears following several pathologies, the most common of which are:
- A degenerative cause (progressive destruction of the white and gray matter of the spinal cord)
- General bacterial and viral infections with localization at the spine (shingles virus, poliomyelitis, chickenpox, tuberculosis, syphilis)
- An infection by a parasite (schistosomiasis for example)
- A tumoral cause (primary tumor or after metastasis)
- An inflammatory cause (after an injection, after a vaccine)
- Inflammation due to multiple sclerosis
- A blood clotting problem causing difficulty in blood circulation in the spinal cord
- Bleeding in the meninges (arachnoid, dura mater) after use of anticoagulant treatment (anti vitamin K and heparin derivatives)
- Poisoning (by carbon monoxide, mercury, lead, etc.)
- Vitamin B12 deficiency
- A surgical intervention at the level of the spinal cord
More rarely, the myelopathy can occur as a result of:
- An experienced management herniated disc
– Inflammation of the spine (ankylosing spondylitis, rheumatoid arthritis)
The rest of our article will focus more on the cervicarthrotic myelopathy.
What is cervicarthrosic myelopathy or degenerative cervical myelopathy?
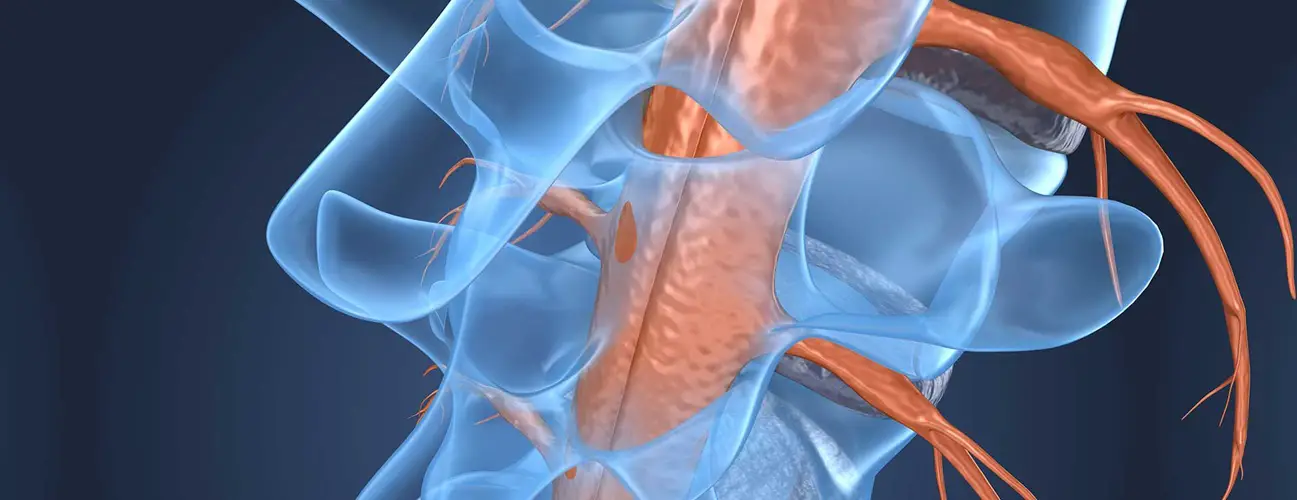
La cervicarthrotic myelopathy is caused by aging and is therefore found in the elderly. Osteoarthritis changes related to aging vertebrae with age lead to a narrowing of the cervical canal through which the spinal cord.
Indeed, aging leads to changes in the bone, ligament and disc structures of the cervical spine. These modifications affect the posterior joints of the rachis which enlarge as well as the intervertebral discs which weaken and deform. The ligaments, on the other hand, thicken. All these anatomical changes lead to a decrease in the diameter of the Spinal canal. The spinal cord contained in this channel is therefore chronically compressed, including with the nerve roots.
Symptoms of the disease
The symptoms of myelopathy, especially cerviocarthrosic, appear as the lesions of the spinal column are formed. They can therefore evolve over several months. Sometimes these symptoms can be triggered by neck trauma or sudden movement of the neck. We find :
- A spinal syndrome which is manifested by pain in the cervical region (cervical myelopathy) dorsal or lumbar (dorsal and lumbar myelopathies), spontaneous or provoked by palpation. There is also stiffness and deformities next to the portion of the spine affected.
- Un injury syndrome due to the compression of the nerve roots by the deformations of the anatomical elements of the spine. This is pain and paresthesia (tingling, tingling) in one or both arms. They may be accompanied by motor disorders, an abolition of one or more neurological reflexes, amyotrophy (muscle wasting), cramps, spontaneous and irregular contractions of muscles at rest (muscle fasciculations). However, it should be noted that sensory disorders are rarer.
- Un sublesional syndrome due to the suffering of the nerve roots that pass through the spinal cord, manifested by:
- Motor disorders: claudication, motor disorders of the lower limbs, bilateral Babinski sign, osteotendinous hyperreflexia (exaggeration of reflex responses during the neurological examination), stepping (particular gait where the tip of the foot is constantly lowered or the patient drags the foot on the ground).
- Sensory disorders, which vary according to the topography of the myelopathy.
In general, these abnormalities are bilateral, with no real upper limit.
- sphincter disorders : In myelopathy, they are moderate and occur late. One can observe imperative urination (urgent need to urinate or even urinary incontinence) dysuria (discomfort or pain when the patient urinates).
Babinski's sign
Babinski's sign (or plantar skin reflex) Is used in neurological examination to detect a possible lesion of the central nervous system (brain and marrow spinal). It consists of stimulating the sole of the foot using a pointed object from the heel to the toes from the outside to the inside of the foot.
The normal reflex response (when there is no neurological involvement) is a flexion of the toes, the big toe moving towards the ball of the foot and the arch of the foot arching. In case of proven neurological lesion, there is a majestic extension of the big toe with the spacing of the other toes.
Diagnostic
Diagnosis is determined by the presence of at least one symptom of each of the triad syndromes spinal syndrome-lesional syndrome-sub-lesional syndrome ou sphincter disorder.
Magnetic resonance imaging is the test of choice for diagnosing myelopathy. This paraclinical examination makes it possible to visualize the spinal cord and the nerve roots in relation to the cerebrospinal fluid. It may show a deformation of the spinal cord.
Computed tomography (scanner) and standard x-rays do not allow to see with precision the spinal cord in order to detect a myelopathy. However, they can objectify indirect signs including dynamic changes in the spine, quality and alignment of the vertebrae.
Electromyography is often done to rule out other neurological disorders. The somatosensory and motor evoked potentials do not constitute examinations for diagnostic purposes but make it possible to assess the functional state of spinal cord.
Treatment: What to do?
Depending on the symptomatology presented by the patient, the treatment of the myelopathy can be done in two ways. If the patient has moderate and not very disabling symptoms, medical and physical treatment should be adopted.
– Resting the spine by wearing a cervical collar or neck brace for example (in case of impairment of the cervical spine)
– Avoidance of activities with a major impact on the spine (arduous household chores, sports) and prescribe a work stoppage if possible
- Kinesitherapy structured and meticulous, gentle massages while avoiding manipulation and traction, especially cervical
– Medicines: painkillers, non-steroidal anti-inflammatories, muscle relaxants, corticosteroids (orally or by infiltration). If the cause of the myelopathy is an infection, it will require antibiotic treatment.
– Monitoring the patient in order to detect signs of worsening of the disease as early as possible. myelopathy
– Inform the patient about the risk factors that can lead to an aggravation
If the patient presents with severe and debilitating symptoms, the patient should be offered surgery:
- Do a laminectomies when several spinal levels are affected to widen the spinal canal
- Do a discectomy ou arthrodesis in case of impairment limited to only one or two spinal levels
– Make a reduction of osteophytes
Conclusion
La myelopathy is the name given to any pathology of the spinal cord. All portions of the spinal cord can be affected but the most serious topographic form is the cervical myelopathy. The most common cause of cervical myelopathy is that due to aging called cervicarthrotic myelopathy.
The clinical picture is variable, ranging from mild dysfunction, such as numbness or dexterity problems, to severe dysfunction, such as paralysis and urinary disorders. The finding of limb paresthesia should therefore not be ignored by patients and healthcare professionals.
Magnetic resonance imaging should be done to make the diagnosis. Medication and physical means are the rule in case of non-invalidating signs. Surgery will be done in case of severe symptoms.
Rest and supervision must be required.