Article reviewed and approved by Dr. Ibtissama Boukas, physician specializing in family medicine
Back pain is common, and can be caused by many different factors. One of the often overlooked causes of low back pain is cluneal neuralgia, a condition where the cluneal nerves are irritated or compressed. Moreover, a wrong diagnosis can lead to ineffective treatments, sometimes even going as far as surgery.
This article explains the causes and symptoms of cluneal neuralgia to guide towards this diagnosis. Also, therapeutic modalities will be proposed to relieve pain and improve quality of life.
Definition and anatomy
Neuralgia is a medical term used to describe severe pain, often throbbing or burning, along a nerve path.
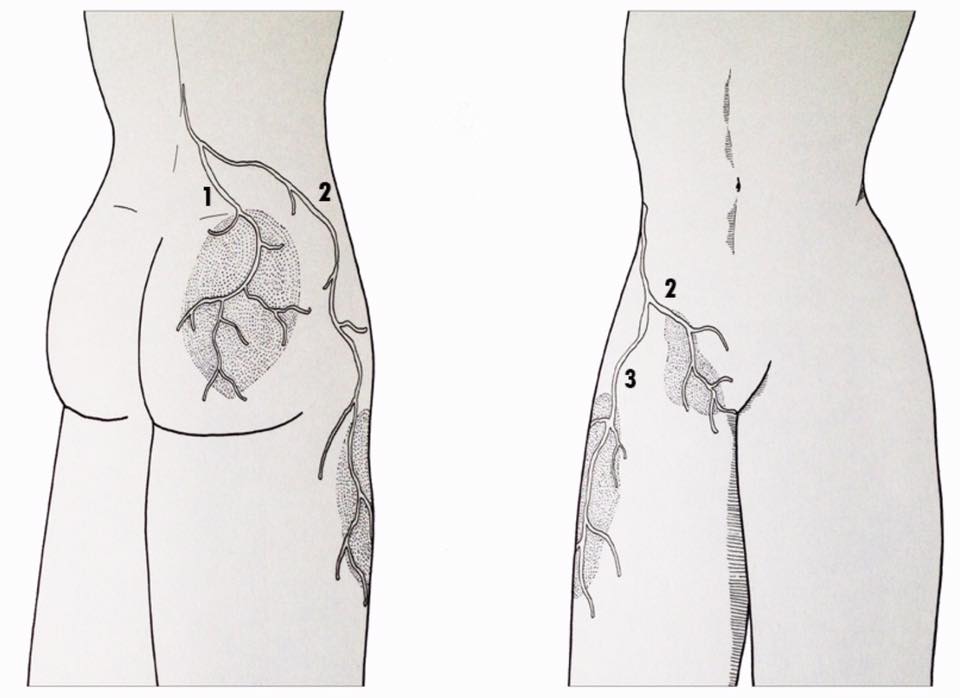
The cluneal nerves (separated into cluneal nerve lower, middle and superior) are cutaneous nerves, that is, they provide sensation to the skin surrounding the buttocks. Specifically, the inferior cluneal nerve innervates the lower part of the buttocks, the middle cluneal nerve innervates the middle part, and the superior cluneal nerve is responsible for providing sensation to the upper part of the buttocks. It should be noted that these nerves do not have a motor role (they do not allow movement).
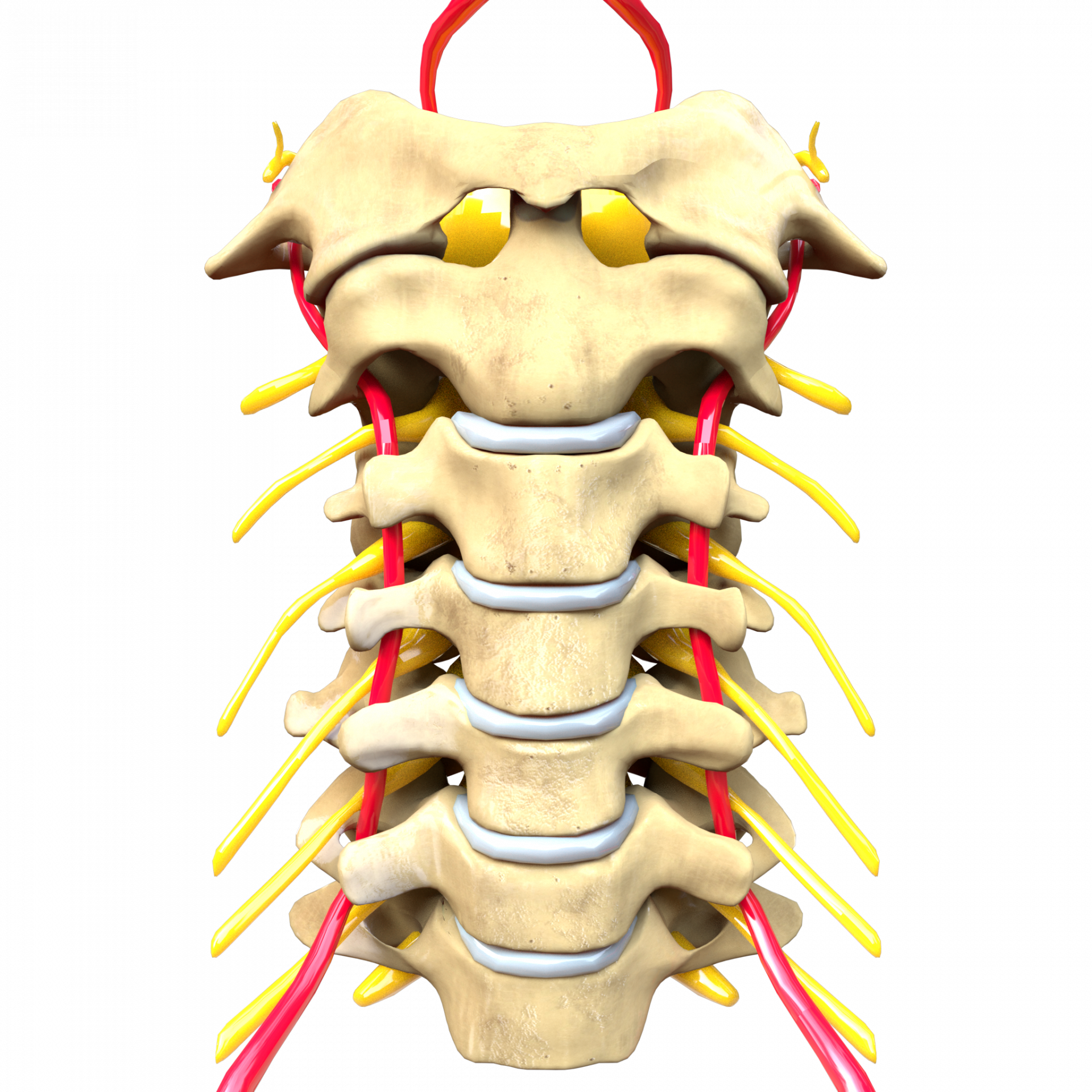
Of the cluneal nerves, the superior and inferior are generally most at risk of compression. The branches of the superior cluneal nerve depart from the spine, pass through the posterior region of the pelvis and descend into the buttock. It is at the level of the upper edge of the pelvis that these branches can be compressed or irritated.
The branches of the inferior cluneal nerve, on the other hand, cross the lower part of the buttock, just above the ischial tuberosity (the seat bone). They can be compressed and irritated by a sudden fall on the buttocks or by prolonged sitting on a hard surface, especially if the gluteal muscle is not developed enough to cushion the impact. Another potential area of conflict is at the sacrotuberous ligament.
Cluneal neuralgia mainly affects women between the ages of 55 and 68, although it can also affect young and active populations. (Source)
Causes
Essentially, the pain caused by cluneal neuralgia is due to the irritation or compression of the cluneal nerves, causing an inflammatory phenomenon responsible for the symptoms.
As mentioned previously, this nerve irritation can occur in the nerve path of the cluneal nerve. Most often, it is done at the level of the iliac crest (upper branch of the cluneal nerve), although it may also lie below the long posterior sacroiliac ligament in some cases (innervation of the middle branch of the cluneal nerve).
What can cause this nerve irritation of the cluneal nerve? Some of the elements potentially responsible for cluneal neuralgia include:
- disc protrusion et herniated disc
- Degenerative disc disease
- Maigne syndrome
- Unsuitable and/or prolonged postures.
- obesity
- Metabolic or hormonal changes
- Underdeveloped gluteal muscles
- Abdominal weakness
- Trauma (such as a fall on the buttocks)
- Spine surgery where the removal of bone grafts can affect the cluneal nerves.
- Scar tissue (post-operative)
Symptoms of the disease
The main symptom of cluneal neuralgia is pain in one or more of the following areas:
- Lower back
- The buttocks
- The Pelvis
- The perineal region
- Oldest boy
- Thigh
- The upper part of the calf
In general, the pain is exacerbated by lumbar movements such as extension, flexion, or rotation of the trunk. Prolonged static postures and walking also aggravate symptoms.
Diagnostic
The diagnosis of cluneal neuralgia is difficult to make due to the similarity of symptoms with other conditions. We think in particular of:
- zygapophyseal osteoarthritis
- the syndrome iliolumbar ligament
- la sciatica
- la cruralgia
- toute radiculopathy
- any discopathy
- a dysfunction sacroiliac
Tests usually include a physical exam, particularly of the gluteal region and iliac crest. For example, a derivative of Tinel's sign can be elicited by stimulating the cluneal nerve in the buttock. Patients then experience characteristic pain and numbness in the affected area.
As the cluneal nerve is purely sensory, hyposensitivity may also be noted in the gluteal region.
The cluneal nerve being very fine (diameter between 1 and 3 mm), themedical imaging may not provide useful diagnostic information. It is therefore not uncommon to encounter negative results on the scanner, magnetic resonance imaging (MRI) or other.
If cluneal neuralgia is suspected and characteristic symptoms have been elicited by stimulating the cluneal nerve, then an anesthetic injection can be used at the painful site to see if the symptoms resolve. If so, the diagnosis can then be confirmed and treatment directed accordingly.
Treatment
On the one hand, medical treatment with specific drugs can be implemented to relieve the symptoms. These include anti-inflammatories, pain relievers, muscle relaxants and/or anti-epileptics.
Advice related to weight loss can be given if it is felt that being overweight would contribute to the symptoms. Likewise, avoiding wearing a belt or tight clothing could avoid unnecessary stress on the cluneal nerve.
Mobilizations or massages from a qualified therapist (physiotherapist, osteopath, chiropractor, etc.) can also release nerve pressure and relieve symptoms in some cases. In addition to these manual techniques, there are other analgesic methods aimed at reducing pain and improving quality of life (electrotherapy, acupuncture, etc.).
Certain trunk stabilization exercises (sheathing and others) could be prescribed by a physiotherapist if it is estimated that a lumbar instability contribute to the clinical picture. The " Prone Instability Test“, although it is not completely reliable, makes it possible to put forward segmental hypermobility suggestive of potential instability.
A nerve block may also prove helpful, especially if it has provided significant relief for diagnostic purposes. On the other hand, the results are mixed, and the success rate varies enormously depending on the individual. It should be noted that a single infiltration is sometimes insufficient, and that it is not uncommon for the doctor to recommend up to 3 infiltrations if he is convinced that the cluneal nerve is responsible for the symptoms.
If cluneal neuralgia is believed to be due to instability of the spinal ligaments (such as the posterior sacroiliac ligament), the prolotherapy may be a treatment option aimed at stabilizing the area.
In patients with cluneal neuralgia whose pain is not relieved by conservative treatment, surgery may be an alternative option. Nerve decompression under general or local anesthesia and rhizolysis are the methods of choice.
Projects
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5944640/
- https://www.apollopainman.com/blog/benefits-of-cluneal-nerve-stimulation