Article reviewed and approved by Dr. Ibtissama Boukas, physician specializing in family medicine
What is spinal cord stimulation, and how can it help you if you ever suffer from chronic pain? Does this treatment technique present any risks? How is recovery going? This popularized article explains everything you need to know about this modality used in the treatment of stubborn pain.
Definition
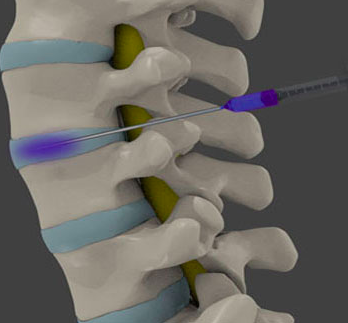
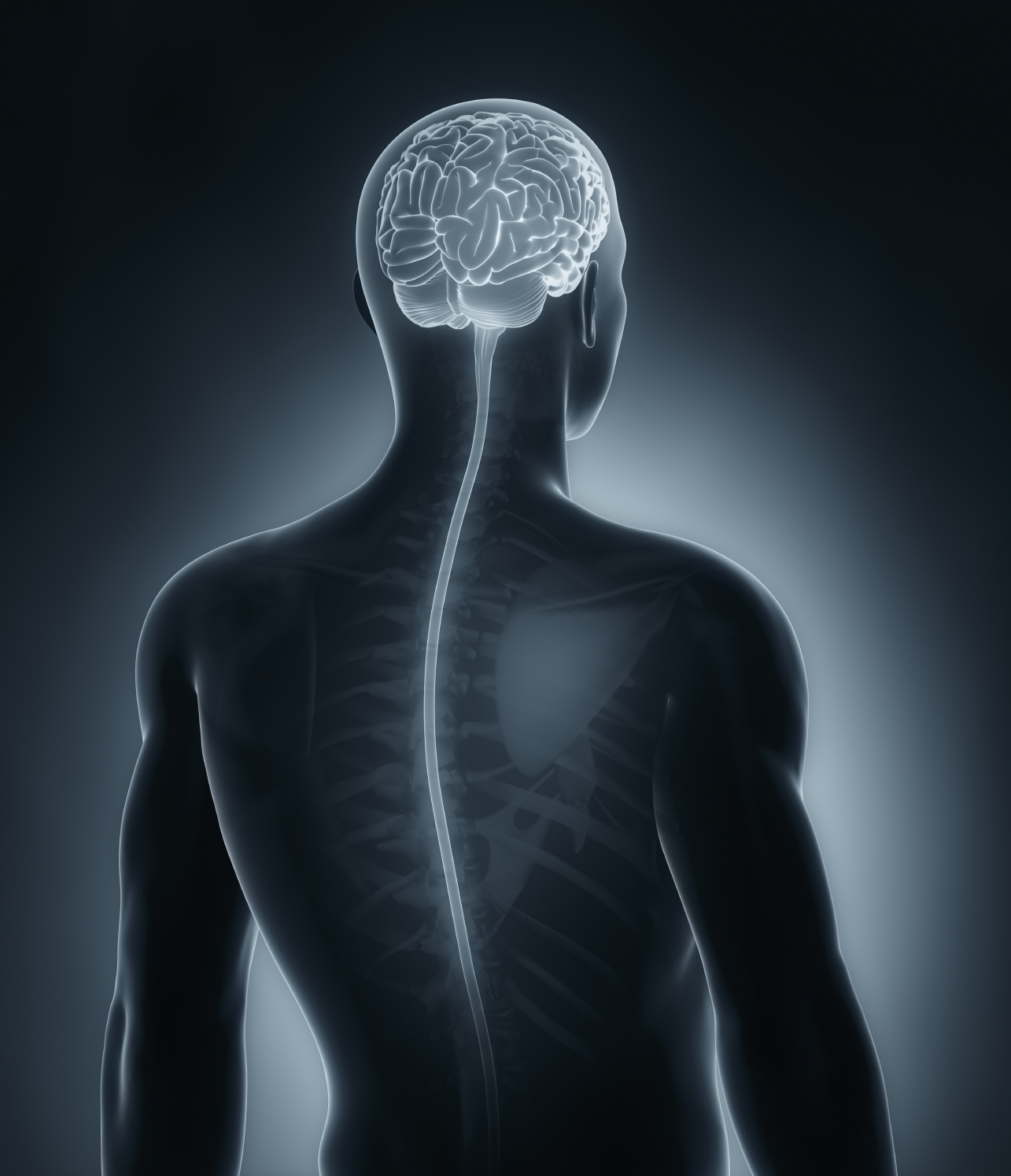
Spinal cord stimulation is a minimally invasive interventional technique used in the management of chronic pain. Its objective is to "short-circuit" an area of stubborn pain of neuropathic origin by sending electrical stimulation to the spinal cord using electrodes.
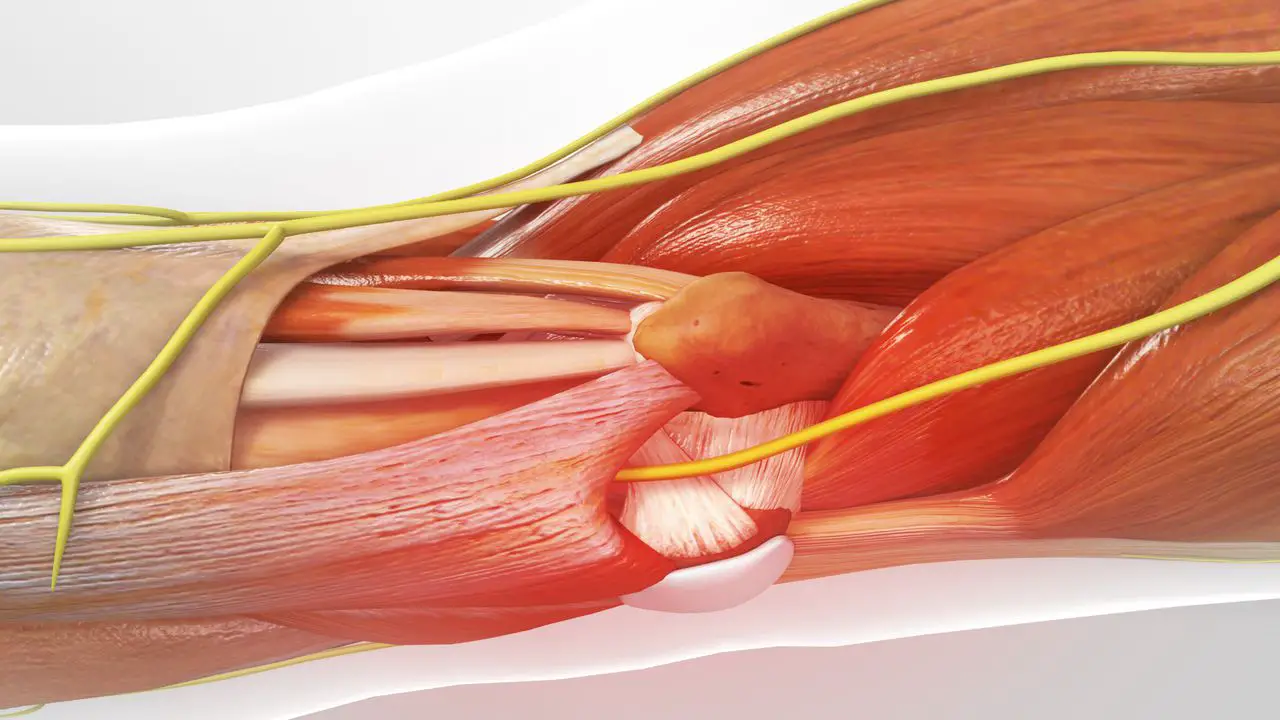
Based on the “Gate Control” theory of Wall and Merzack, these stimulations in the form of paresthesias would have the effect of blocking the painful message traveling to the brain, thereby providing a reduction in symptoms.
These electrodes are connected to a pulse generator implanted in another region of the body (abdominal or buttock region).
Indications
The indications most commonly encountered in the literature are as follows:
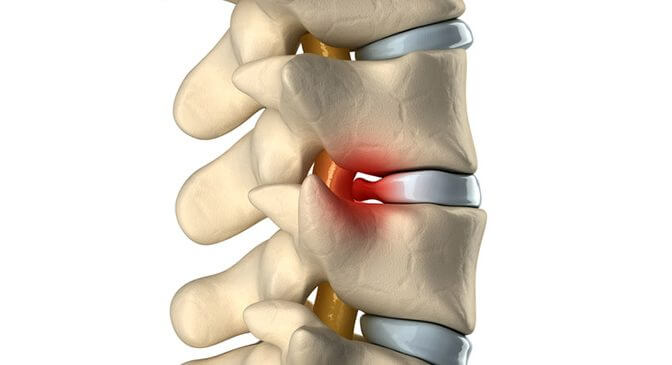
The failure syndrome spine surgery
This condition presents as residual pain in the lower back (which may include pain radiating down the leg) that persists after one or more spinal surgeries.
The syndrome complex regional pain
Complex regional pain syndrome manifests as pain in one extremity. It may be accompanied by edema, or vasomotor or sweating alterations. Although it can appear spontaneously, it usually occurs after trauma or surgery.
Critical limb ischemia
Ischemic pain appears when an organ is no longer sufficiently irrigated to meet its metabolic needs. It is found mainly in patients over 55 years of age, and is often due to the progression of arteriopathy.
Angina refractory breast pain and refractory cancer pain.
Both of these conditions frequently cause chronic pain, and could benefit from spinal cord stimulation.
Procedure
The placement of a neuro-stimulator is done in 2 steps:
The first step consists of placing percutaneous electrodes under neuroleptanalgesia, which is less invasive and allows ideal positioning of the electrodes (waking up the patient per procedure).
The electrodes are connected to an external generator; It is sometimes necessary to put electrodes under general anesthesia by surgical means (failure of the percutaneous technique, repositioning, etc.).
The test phase lasts on average one week and must include a return home. It is considered positive if the patient indicates a level of relief greater than 50% and comfortable stimulation, covering at least 80% of the painful area.
The second step then consists in positioning the generator in the abdomen and connecting it to the electrodes. The doctor can make the settings using a programmer that communicates with the generator.
The patient has a remote control to turn the device on/off and adjust the intensity.
Risks and Complications of Spinal Cord Stimulation
Complications occurring after placement of a spinal cord stimulator are of three types:
Biological complications: infection, hematoma and leakage of cerebrospinal fluid (LCR);
hardware complications: lead migration, lead or extension fracture, implanted neurostimulator disconnections and malfunction;
As for the side effects related to implantation or stimulation, there are:
- pain at the implant site of the pacemaker
- loss of effectiveness over time
- unpleasant sensations (uncomfortable paresthesias).
Only infections andepidural hematoma (exceptional) should be considered severe complications. The infection (at Staphylococcus epidermidis ou aureus in 48% of cases) necessarily requires removal of the material, and generally 8 days of antibiotic therapy. The material is then rested at least two months after infection.
Convalescence
Recovery after neuro-stimulation takes a period of between 2 to 8 weeks.
Post operative instructions
After the operation, it is recommended:
- apply ice to the wound for 24 hours to reduce swelling and pain;
- administration of analgesics to reduce the pain of the procedure, and antibiotics to prevent infections.
You may feel pain where the neurostimulator is implanted for two to eight weeks after the procedure.
This pain is caused by the tissue healing process and occurs with all types of surgical implantation. This is your body's natural response to the implant.
Your doctor may recommend that you restrict your activities during this time. You may need to avoid lifting, bending, or turning.
This will allow time for scar tissue to form, which will help secure the probe. Even after six to eight weeks, still be careful when performing these types of movements.
Continuing care
Discuss with your doctor which activities you can do without problems, and which ones you should take a little more care about. Contact your doctor immediately if you:
- experience additional or unusual pain;
- notice changes in the effects of pain treatment.
Expected results of spinal cord stimulation
A study conducted by PROCESS compared epidural spinal cord stimulation to conventional medical management in a group of chronic pain patients; 93% of Epidural Spinal Cord Stimulation patients said that "based on their experience to date, they would be willing to start treatment again."
We find a return to work in 15% of epidural spinal cord stimulation versus 0% of conventional medical treatment
The PROCESS study found 32% complications (10% electrode migration, 8% infection or breakage, 7% loss of paresthesias), of which 24% required reoperation. VSComplications occur mainly in the first 3 years, are benign and reversible, and do not affect adherence to treatment.
Cost studies show that the spinal cord stimulation technique is more profitable after 2,5 years compared to conventional medical care.
Conclusion
Spinal cord neurostimulation is a simple technique for placing a neuro-stimulator generally implanted under the skin of the abdomen or the buttocks region; it generates “therapeutic” paresthesias in the painful area with the aim of reducing pain.
Spinal cord stimulation has a significant but minor adverse event rate. These complications must be put into perspective when we know that the rate of pain relief is 50% in two thirds of patients suffering from neuropathic pain chronicles. The overall satisfaction rate is around 85%.
Patients for whom spinal cord stimulation is indicated must be selected at all costs, otherwise the treatment will probably end in failure. Discuss with your doctor if you ever suffer from chronic pain and consider this procedure.
Sources
Mark the Bishop, pain surgery, Springer-Verlag France, 2014
Kumar and all, Spinal cord stimulation versus conventional medical management for neuropathic pain: A multicentre randomized controlled trial in patients with failed back surgery syndrome, Pain 132, 2007, p 179–188.
Marc Leveque, pain surgery, Springer-Verlag France, 2014
Denys Fontaine, Spinal cord stimulation: indications and results, Elsevier Masson, 2011
Camberlin C, San Miguel L, Smit Y, Post P, Gerkens S, De Laet C. Neuro-modulation for the management of chronic pain : implanted spinal cord stimulation systems and analgesic intrathecal pumps - Synthesis.