Article reviewed and approved by Dr. Ibtissama Boukas, physician specializing in family medicine
Your doctor has decided to give you an x-ray to identify the source of your back pain. The results of the imaging report mention spondylolisthesis. We are talking about grade 1, 2, 3, L4-L5, L5-S1, spondylolysis, or possibly pars interarticularis or anterolisthesis…
In short, this a priori complex diagnosis (seeing the name!) worries you. And you would like to better understand your condition. Is this the cause of your back pain? Can spondylolisthesis be treated? Are there natural exercises and treatments that could avoid surgery?
In the following article, we cover everything you need to know about spondylolisthesis, with an emphasis on simple and practical concepts. You will leave with a better understanding of your condition, as well as concrete tools to help you in the treatment of your back problem.
Definition
Simply explained, a spondylolisthesis is a slipping of vertebrate.
I can already see you panicking reading the previous lines. You probably imagine displaced vertebrae or staggered which must at all costs be put back in place via manipulation. (Keep reading, you will have all your questions answered!)
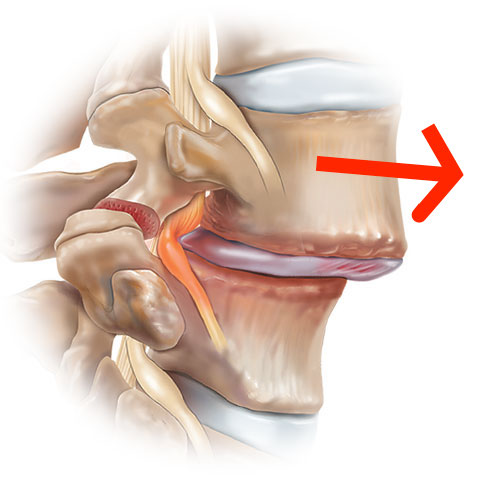
This slippage can appear at all levels, but the lumbar levels L5-S1 (and then L4-L5) seem to be the most affected by spondylolisthesis. For example, L4-L5 anterior spondylolisthesis (anterolisthesis) means that the L4 vertebra has slipped forward relative to the vertebra just below (L5).
The causes of spondylolisthesis
There are 3 types of spondylolisthesis, each type having a well-defined cause:
1- Isthmic spondylolisthesis
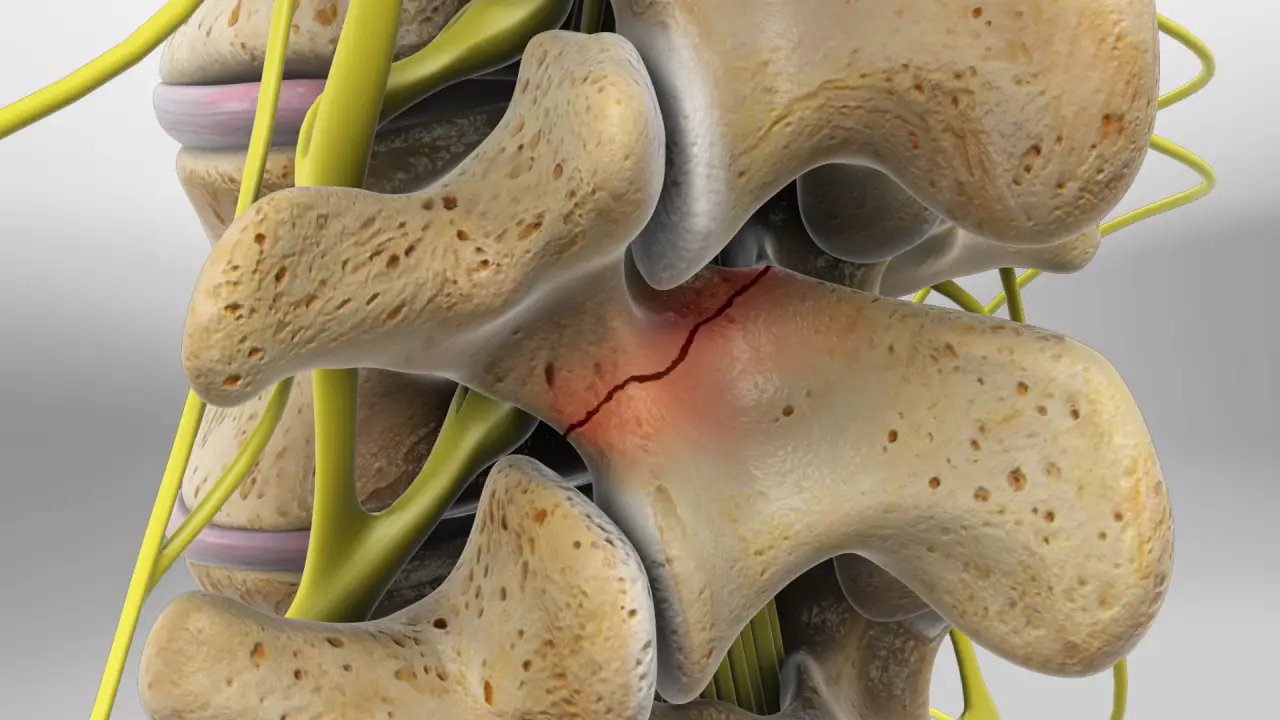
To understand isthmic spondylolisthesis, one must first be familiar with spondylolysis. The latter corresponds to a fracture of the isthmus, a bony bridge connecting one vertebra to another.
This is a more common condition than you might imagine, affecting between 4-8% of the population. And since it can be asymptomatic, it is often detected by chance during an X-ray examination of the back.
Although this fracture can be traumatic, it is mainly progressive (called a stress or fatigue fracture), and is present in young athletes – especially men – practicing sports that favor lumbar extension.
These include ballet, gymnastics, weightlifting, diving and swimming. Carrying a heavy backpack in children could possibly be a causal factor, although the link between backpack and low back pain is not clear.
The consequence of isthmic spondylolisthesis is an advancement of the vertebra and a lumbar instability due to the defect at the level of the vertebral isthmus.
2- Degenerative spondylolisthesis
In the case of degenerative spondylolisthesis, it is the wear of intervertebral discs and osteoarthritis which are responsible for the slippage of vertebrae.
As the height between the vertebrae decreases, it is not uncommon to observe associated discopathies (such as disc pinching, herniation or disc protrusion).
Certain factors such as menopause and osteoporosis can promote degenerative spondylolisthesis. Moreover, degenerative spondylolisthesis is much more present in women.
3- Dyplastic spondylolisthesis
Much rarer, dysplastic spondylolisthesis is congenital and affects women more.
It comes from a malformation of the vertebra at birth. For example, the isthmus there is abnormally elongated, or the articular facets have an abnormal alignment.
The diagnosis and the different grades of spondylolisthesis
Chances are you have already been diagnosed with spondylolisthesis. If not, how to detect this condition? Through a review by medical imaging.
There are no clinical tests that can diagnose this condition. One can note a exaggerated lumbar lordosis, or even an elevation in the lower back in more severe cases (Step Off Sign). But more often than not, the consequences of spinal slippage will mostly be observed during the clinical evaluation (explained in the next section which discusses the symptoms of spondylolisthesis).
To actually identify spondylolisthesis, a lumbar x-ray enough. A scanner can also be prescribed to better visualize bony structures, and an associated isthmus fracture. On the other hand, if we wish to have more diagnostic information (for example, identify the affected nerve roots, or quantify the narrowing of the spinal canal), a IRM will be necessary.
In imaging, we often use the Meyerding classification to quantify the vertebral slippage specific to spondylolisthesis. More precisely, we rate the advancement of a vertebra in relation to the underlying vertebra via grades:
Grade 0: In this case, there is no forward slippage of the vertebra. On the other hand, there can be spondylolysis, as long as it is stable and fixed.
Grade 1: Here there is a slip of less than 25% of the size of the vertebral endplate. This type of grade 1 spondylolisthesis is very common, and accounts for almost 3/4 of spondylolisthesis cases.
Grade 2: The slip is located between 25% and 50% of the size of the vertebral endplate. We are starting to talk about lumbar instability in this situation.
Grade 3: The slip is located between 50% and 75% of the size of the vertebral endplate. Lumbar instability is observed in this situation.
Grade 4: The slippage is located between 75% and 100% of the size of the vertebral endplate.
Grade 5: Here, the shift is complete. It's called spondyloptosis. The vertebra is so advanced that it is placed in front of the sacrum.
Note: There are other classifications to quantify the vertebral slippage caused by spondylolisthesis. Taillard's index separates slippage into 4 grades.
Depending on the grades of spondylolisthesis, one could observe different symptoms. Management will be adapted to the grade, but also (and above all) to the patient's symptoms.
Symptoms of spondylolisthesis
What if I told you that spondylolisthesis is sometimes asymptomatic? This means that some people with no lower back pain have spondylolisthesis without even knowing it.
On the other hand, it can happen that spondylolisthesis is symptomatic. This is probably the reason that prompts you to inform yourself about this condition. The symptoms actually depend on the irritation caused by the slipping vertebra (either an inflammatory process, nerve irritation, etc.).
The most common symptom is pain. Low back pain appears either gradually, in the form of morning stiffness, or is manifested by recurrent lumbago.
In cases of advanced spondylolisthesis, there is often an increase in symptoms when the trunk is extended, that is, when the trunk is straight (for example, when standing or walking).
Conversely, the leaning forward position seems to relieve symptoms, in particular because it opens the lumbar canal. It is for this reason that some patients with spondylolisthesis can cycle without any problem, and have no pain when leaning on their Shopping Cart in the supermarket (the shopping cart sign refers precisely to the reduction of pain in the position of lumbar flexion).
In addition to leaning forward, lying on your back can also relieve symptoms. This is because this position decreases lumbar instability and provides support for the lumbar region.
If a nerve (or a nerve root) is irritated, then neurological symptoms such as tingling, numbness, weakness, radiation and feeling of electric shocks in the legs are observed. Spondylolisthesis may be responsible for sciatica or an cruralgia.
In severe cases, for example when the slippage is significant, the vertebral canal can also be affected. We can then observe a narrow lumbar canal (spinal stenosis) causing in particular intermittent claudication, or even cauda equina syndrome.
In any case, these conditions represent medical emergencies.
Treatment: What to do?
To treat spondylolisthesis (and any other forms of low back pain), there are 2 types of treatments: conservative and invasive.
A doctor (or a back specialist) is often consulted in the first line to assess and treat spondylolisthesis. Among other things, it is possible to see your general practitioner, a rheumatologist, an orthopedist, a neurosurgeon, etc.
Conservative treatments only address the source of the problem, and further correct the consequences of spondylolisthesis. For example, the objective will be to reduce pain, reduce nerve irritation, maximize trunk stability and promote a healthy lifestyle.
Invasive treatments are generally used as a last resort, when conservative treatment has failed, or if there is a medical emergency.
Conservative treatments
Conservative treatments include:
Medication
Although it won't correct the cause of spondylolisthesis, medication can be helpful in controlling symptoms.
The doctor often starts with a prescription of anti-inflammatory, painkiller and/or muscle relaxants to control the symptoms.
In the case of neuropathic pain (for example, radiation in the leg associated with numbness and tingling), the doctor may prescribe anti-epileptics such as Lyrica.
In cases of severe pain, it is possible to resort to anti-depressants, oxycodone, codeine, morphine and its derivatives, etc.
Footnotes: For more information on the choice of medication for his back pain, consult next article. On the other hand, know that it is imperative to follow the recommendations of your doctor. He will know how to choose the right drugs, and adjust the doses according to the medical history and the patient's condition.
Rehabilitation and therapy
Un physiotherapist (physiotherapist) can guide you through an exercise program aimed at toning the stabilizing muscles of the trunk, and correcting muscle and joint imbalances potentially responsible for your symptoms.
As mentioned, some cases of spondylolisthesis will be relieved by lumbar flexion exercises which will aim to open the lumbar canal.
In addition, it is not uncommon to observe a retraction of the hamstrings which can be corrected through stretching exercises.
Active core muscle strengthening work was also demonstrated to be effective in cases of spondylolisthesis.
A frequently asked question concerns hyperextension exercises. Are they to be banned forever, knowing that spondylolisthesis (anterior) causes a forward slippage of a vertebra?
Everything will depend on the patient's symptoms, and the grade of spondylolisthesis. In more advanced grades, it is advisable to avoid hyperextension exercises that arch the lower back, simply to prevent aggravation of the condition.
On the other hand, in the “lighter” cases, it will be necessary to evaluate the movements and determine their impact on the pain. For example, a lumbar extension might be tolerated if it does not worsen the symptoms of a patient with grade 0 or 1 spondylolisthesis.
Besides physio, are there other forms of therapy that can help?
Yes. Other therapists such as bone therapists and chiropractors can also relieve symptoms of spondylolisthesis. For example, they will relax tense muscles and decrease stiffness through manual techniques.
On the other hand, it should be noted that a vertebra anteriorized by spondylolisthesis cannot be put back in place via manipulation (or any other technique).
So, if a therapist promises to replace your vertebra having undergone spondylolisthesis via manipulation, look elsewhere!
Moreover, an advanced and unstable spondylolisthesis (especially if there is spondylosis) constitutes a contraindication to spinal manipulations. In other words, one should not “crack” the lumbar region if the spondylolisthesis is severe!
In addition, spondylolisthesis can sometimes be aggravated by mechanical stress (such as carrying heavy loads repeatedly, especially if you do not have the muscles to tolerate this effort). This could limit you in the practice of your profession, and affect your quality of life and sleep.
With this in mind, an occupational therapist could assess the demands specific to your occupation, and determine if a job adjustment will relieve your symptoms, or prevent the progression of spondylolisthesis. In extreme cases, professional retraining may be considered.
Immobilization by a corset in certain cases
In some cases (such as traumatic spondylolysis, for example), immobilization by corset may be prescribed.
For example, a painful traumatic spondylolysis may require temporary bracing.
In addition, some doctors offer lumbar corsets to their patients suffering from acute pain. Although they may sometimes be necessary, it must be remembered that these corsets come with their drawbacks (especially if used for a prolonged period):
- Lumbar corsets make the stabilizing muscles of the spine weaker (because they no longer need to work)
- They make the back stiffer (because the belt limits full movements)
- They create a phenomenon of dependence and a loss of confidence in one's back
- They limit abdominal and diaphragm expansion, which interferes with breathing.
It is for this reason that many therapists and health professionals have a negative view of these passive supports. Anyway, see these lumbar belts like a crutch you use after a sprained ankle!
Finally, the last resort before surgery (for severe cases) are pain centers and back schools.
What about natural remedies?
Although they are not supported by solid scientific evidence, several natural products and home remedies are used to treat pain related to spondylolisthesis, in particular for their anti-inflammatory power. It is essential to consult a doctor beforehand, mainly to avoid drug interactions and side effects.
Here is a non-exhaustive list of plants and essential oils that are effective in controlling pain and inflammation. It must be understood that these products will not treat the cause of the symptoms, but rather their consequences on a daily basis.
The products are available on the site Country. Use promo code LOMBAFIT15 if you wish to obtain one of the following products, or any remedy aimed at relieving your symptoms and improving your quality of life:
- Turmeric. Thanks to its antioxidant and anti-inflammatory powers very powerful, turmeric is one of the most used plants in a culinary and therapeutic context. The composition of turmeric is essentially made of essential oils, vitamins (B1, B2, B6, C, E, K) and trace elements. But it is to its composition rich in curcumin and curcuminoids that we owe them and calm skin of this spice.
- Ginger. In addition to the special flavor it brings to the kitchen and its aphrodisiac properties, ginger is a root well known for its anti-inflammatory powers. the gingerol gives it its anti-inflammatory action. It is an active component acting on the inflammatory pain related to chronic joint inflammatory diseases, including rheumatoid arthritis, lupus, rheumatic diseases, etc. It has been proven that this active element is also effective in acting on the inflammation linked to arthritis and sciatica. Ginger also has other benefits thanks to its high potassium content and its richness in trace elements (calcium, magnesium, phosphorus, sodium) and vitamins (provitamin and vitamin B9).
- Omega-3s. Omega-3s are polyunsaturated fatty acids that play a very important role in the functioning of our body. They are provided by food in three natural forms: docosahexaenoic acid (DHA), alpha linolenic acid (ALA) and eicosapentaenoic acid (EPA). Beyond their action on the brain and the cardiovascular system, omega-3s prove very effective against inflammation. Indeed, they have the ability to act on the inflammatory mechanisms in osteoarthritis by slowing down cartilage destruction, thus they reduce the intensity of osteoarthritis pain. Sciatica, being most often linked to an inflammation secondary to a herniated disc, it can also respond to omega-3 provided it is consumed regularly.
- Lemon eucalyptus. Eucalyptus is a plant most often used in the form of herbal tea or essential oil. She would have anti-inflammatory effects which give it the ability to act on the bone and joint pain in general and the pain of sciatica in particular.
- wintergreen. Wintergreen is a shrub from which a very interesting essential oil is extracted. It is one of the most used essential oils in aromatherapy. This oil extracted from the shrub bearing the same name, is used in massage to relieve sciatica and act like a analgesic. Indeed, it provides a heating effect thanks to its ability toactivate blood circulation locally.
Remember that these products do not replace medical treatment. Do not hesitate to consult for support adapted to your condition.
Invasive treatments (operation)
In which cases to operate a spondylolisthesis?
First of all, it should be borne in mind that all patients with spondylolisthesis should initially benefit from conservative treatment.
The latter is frequently found to be effective in managing the symptoms of spondylolisthesis, to some extent.
In addition, scientific studies have shown that even if conservative methods fail, the time elapsed in implementing it does not influence the results of surgical treatment.
In other words, there is nothing to lose and everything to gain by trying a conservative approach first !
In the vast majority of cases, patients with spondylolisthesis ask for surgery in the event of refractory pain, that is to say, resistant to all the conservative treatments implemented.
This indication is mainly based on the patient's feelings, on its ability to manage or bear pain (threshold of resistance to pain varies from one individual to another).
In this case (refractory pain), surgery is not an emergency, because there is no immediate risk that threatens the health of the patient. It can therefore be deferred to be carried out calmly after a precise evaluation of all the different parameters.
On the other hand, there are certain situations which require surgical treatment as soon as possible, before the aggravation of the symptoms. Here they are :
- cauda equina syndrome : urinary disorders such as incontinence, loss of sensation in the buttocks and genital area.
- Sciatica paralyzing: pain sciatica with motor disorders in the lower limb which can go as far as paralysis.
- Hyperalgesic sciatica: unbearable sciatic pain despite well-conducted medical treatment.
- Root distribution neurological deficit: loss of sensitivity, motor disorders or pain in an area innervated by a nerve root compressed by spondylolisthesis…
What does the intervention consist of?
The goal of spondylolisthesis surgery is to lift the compression exerted on the nervous elements before fuse the vertebrae to fix them in the correct position thanks a arthrodesis (lumbar arthrodesis, dorsal or cervical).
The union of the vertebrae can call upon a system of rods, de screw and / or cages (osteosynthesis), or to a graft bone (removal of a bit of bone, usually at the level of the patient's hip) which will fuse the vertebrae over time.
In some cases, the displaced vertebra can even be realigned with the rest of the spine.
Sometimes a laminectomies will be necessary to decompress a nervous element.
What is the duration of the intervention?
Surgery for spondylolisthesis is most often done under general anesthesia. It lasts between 1 a.m. and 5 p.m. depending on the techniques used, the complexity of the intervention, the extent of the compression...
For certain spinal procedures lumbar who last less than 2 hours, it is possible to carry out the intervention under spinal anesthesia.
The latter consists of injecting an anesthetic product into the cerebrospinal fluid via a lumbar puncture. This helps anesthetize the lower part of the patient's body. The latter therefore remains aware during the operation, but does not feel no pain.
What is the length of hospitalization?
It is necessary to count 3 to 4 days of hospitalization on average for spondylolisthesis surgery. This duration is obviously variable depending on the complexity of the procedure, the condition of the patient before and after the operation, the stability of the spine, the occurrence of any complications, etc.
What are the possible complications of the procedure?
In addition to classic complications inherent in any other surgery (infection, postoperative hematoma, deep vein thrombosis, pulmonary embolism, etc.), spondylolisthesis surgery can be complicated by:
- Breach of the dura mater: lesion of the envelope that surrounds the spinal cord and its roots with cerebrospinal fluid flow.
- Postoperative hematoma: generally without consequence. Sometimes it can compress the dural bag and its content (spinal cord and nerve roots). In this case, it must be drained quickly to avoid neurological damage.
- Paralysis according to the operated spinal level: for example, in the event of intervention at the level of cervical spine, there is a risk of paralysis of all 4 limbs (tetraplegia).
- Great vessel lesions : they are seen exceptionally when the intervention is done with an anterior approach (the surgeon goes through the stomach to reach the spine, the patient is then lying on his back).
- Damage to an abdominal organ(also anterior).
- Destabilization of osteosynthesis (the vertebrae are not well fixed by the rods/screws/bone graft).
Other complications are possible. Nevertheless, all precautions are taken to make these adverse events exceptional.
How is the recovery period going?
The patient generally sees his symptoms (low back pain, pain in the lower limbs, numbness, etc.) improve gradually in the days or weeks following the intervention.
Sessions of re-education will be necessary to help the patient regain better mobility and flexibility of the back.
He will be able to resume his professional activity after approximately 6 weeks (varies according to profession and condition).
Prognosis: How to live with spondylolisthesis?
You are probably wondering how spondylolisthesis evolves over time. You also want to know how to live with spondylolisthesis. In truth, it is not easy to answer these questions.
Some spondylolisthesis remain asymptomatic for very long periods, even if there is associated spondylolysis. And other spondylolisthesis evolve slowly or quickly depending on factors such as the age of the patient, the origin of the problem, and the grade of spondylolisthesis.
What should be remembered is that a diagnosis of spondylolisthesis is not necessarily a conviction in itself.
Spondylolisthesis and sport
Should we stop exercising when we discover spondylolisthesis? No, not necessarily. If you are able to control the symptoms, there is no reason to stop being active.
On the other hand, as mentioned previously, certain sports that promote extension can accentuate vertebral slippage over time. With this in mind, you should discuss with your healthcare professional to determine whether it is appropriate to make some adjustments to your sports practice.
Weight gain (rapid) can also be a factor favoring the progression of spondylolisthesis. Thus, weight control is ideal if one wants to ensure that the condition does not worsen.
In short, an early diagnosis in order to avoid the potential worsening of the grade of spondylolisthesis remains the optimal solution. Also, monitoring over time via regular X-rays will make it possible to follow the progression of the condition (especially in athletic adolescents).
During this time, it is advisable to remain active as much as possible, emphasizing cladding exercises aimed at stabilizing the lumbar vertebrae and protecting the back. It is important to avoid aggravating the symptoms during movement so as not to overload the lumbar vertebrae and accelerate vertebral sliding.
In the event that the symptoms limit the work, it is advisable to discuss with its doctor the possibility of recognition of handicap. In addition, some adjustments could be made at work to protect the lumbar region and act in prevention.
Conclusion
So much for spondylolisthesis! If ever your doctor has given you this diagnosis, the first reflex is to determine its grade, and the associated symptoms. These elements are even more important than the diagnosis itself!
In addition, your doctor and therapist will be able to prescribe the corresponding treatment to relieve your pain and prevent the progression of spondylolisthesis.
Remember to start with a conservative treatment before considering any more invasive intervention (such as infiltration or surgery).
Movement and exercise are not always contraindicated, and can even help tone the core muscles and thus limit the progression of the condition. A physiotherapist or physiotherapist will be able to guide you at this level.
To conclude, the diagnosis of spondylolisthesis is not a condemnation in itself. There is always something to do to get better, you just need to be well guided, to be patient and persistent.
Good recovery!