Article reviewed and approved by Dr. Ibtissama Boukas, physician specializing in family medicine
Subdural hematoma is the most common intracranial hemorrhage occurring after trauma. It is therefore important to talk about it because it can sometimes go unnoticed, occurring at a distance from the trauma.
This article provides the necessary information to know everything about acute and chronic subdural hematoma, the different causes in adults and children, the symptoms, the means for making the diagnosis, the treatment as well as the possible sequelae and the prognosis.
Good reading !
Definition and anatomy
Definition
Subdural hematoma (HSD) is an effusion of blood that ends up in the space between the external meninges (dura mater) and the intermediate meninges (thearachnoid) of the brain. It usually occurs following a head trauma. We distinguish acute subdural hematoma (HSDA) and chronic subdural hematoma (HSDC).
Acute subdural hematoma is clinically manifested by characteristic signs just after the head trauma. Chronic subdural hematoma, on the other hand, is expressed by symptoms that appear slowly. In this case, the collection of blood between the two meninges builds up over several weeks or even months. This is often due to minimal trauma, which has not been realized.
Anatomy
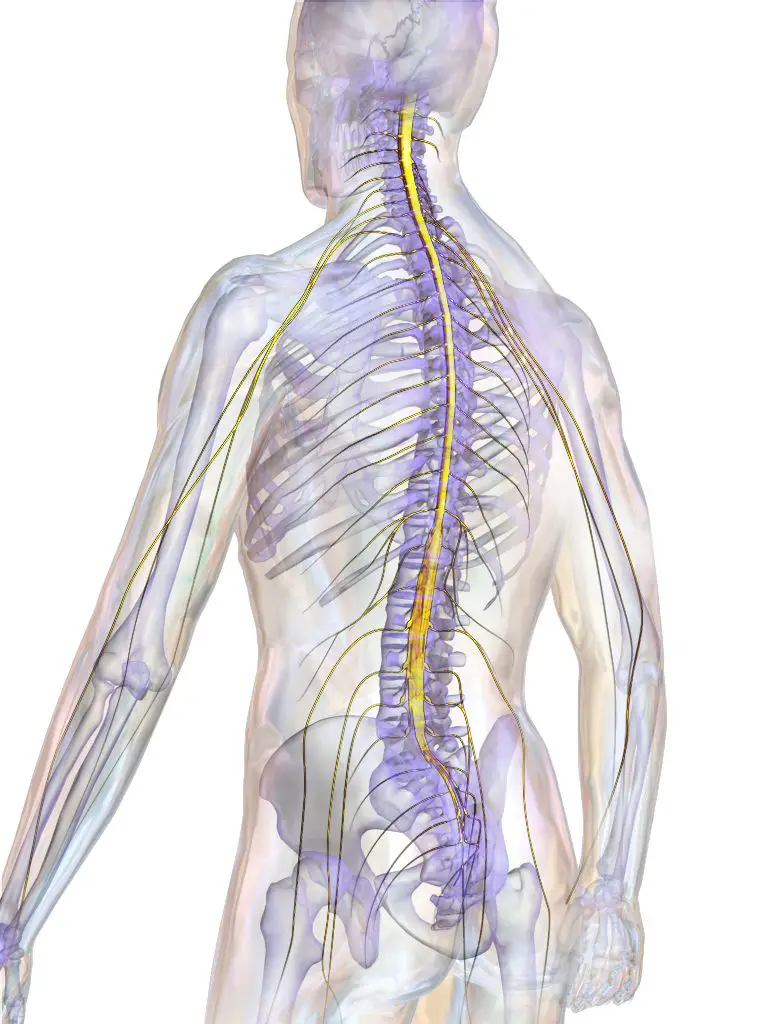
The central nervous system (brain and spinal cord) is surrounded by three membranes called meninges, forming a thick cylindrical sheath. The dura mater is the outermost meninge, then comes the arachnoid, the intermediate meninge and then the pia mater (internal meninge).
The space between the dura mater and the arachnoid is called the subdural space and is the one affected by the subdural hematoma as its name suggests. On the other hand, the space outside the external meninge (dura mater) is called the extra dural space and the space between the pia mater and the arachnoid is called the subarachnoid space. In this last space, the cerebrospinal fluid (CSF) or cerebrospinal fluid (CSF) circulates.
The meninges essentially play a protective role for the brain during head trauma, for example. They allow veins and arteries to pass to the brain and contribute to its nutrition.
In the vast majority of cases, acute subdural hematoma (ASDA) occurs after the rupture of one of these veins crossing the subdural space (anterior or posterior temporal vein, emissary vein, superior longitudinal sinus vein) or of an artery. It can also be bleeding from a focus of contrition in the brain during the cranio-encephalic trauma. In this case, the subdural hematoma is associated with tissue destruction, an ischemic focus (arrest or insufficiency of blood circulation) or blood clots.
Causes
The main cause of a subdural hematoma is head trauma occurring in several circumstances. The most common context is a road accident. A head injury can also occur during a fall on its own height (in the elderly for example in the shower).
There is a predominance ofsubdural hematoma especially chronic in subjects who have certain risk factors, namely: alcoholics, older people and people taking drugs that thin the blood (anticoagulants or antiplatelet drugs).
Another common cause ofsubdural hematoma in children under six months is the shaken baby syndrome. As its name suggests, this syndrome occurs when a baby is shaken by holding it by the trunk, shoulders or limbs. The baby's head is then thrown violently in all directions, which can cause bleeding inside the skull, including the hematoma subdural.
Symptoms of Subdural Hematoma
Symptoms of a subdural hemorrhage start slowly but can appear within minutes. These symptoms are those of intracranial hypertension (HIC or HTIC) essentially. Indeed, the effusion of blood in the subdural space exerts pressure on the brain and the cranial box since the latter is inextensible. There may be a risk of brain damage if the bleeding is severe.
Depending on the degree of severity, the patient with a subdural hematoma may experience headache (headache), dizziness, nausea or vomiting or anorexia (lack of appetite). The patient may also experience spatiotemporal confusion (he no longer recognizes the date of the day or the place where he is), amnesia (no longer remembers his name) or lethargy (abnormal state of deep sleep or extreme attenuation). He may even have seizures (violent and involuntary contractions of all the muscles of the body).
The patient may also present with other signs related to the suffering of the brain, such as paralysis of half of the body. This paralysis occurs on the side opposite the brain injury. Other signs of brain damage are:
- Behavioral Disorders,
- speech disorders,
- Difficulty walking (ataxia),
- Irregular breathing.
- Hearing and sight can be affected by types of diplopia (seeing objects twice) and strabismus (deviation of the axis of one eye).
In infants with shaken baby syndrome, signs ofintracranial hypertension are also present as in adults. It is in the baby an increase in the cranial circumference and a tense fontanel. Other symptoms are:
- Irritability (baby cries),
- refusal to breastfeed,
- Vomiting (the baby is no longer gaining weight properly),
- Alertness disorders such as drowsiness, lethargy, loss of consciousness,
- Seizures,
- Difficulty breathing,
- Respiratory stop.
Diagnostic
Before asking for paraclinical assessments, the medical specialist makes an interrogation, especially with regard to thechronic subdural hematoma which occurs remotely from the trauma. The specialist will look for a context of recent head trauma with the notion of a loss of consciousness or a behavioral disorder.
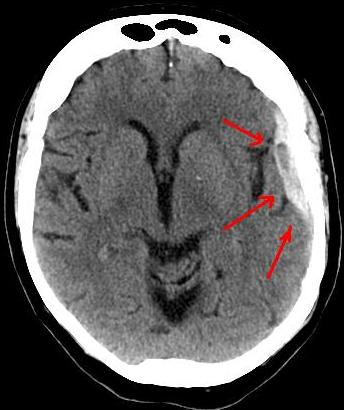
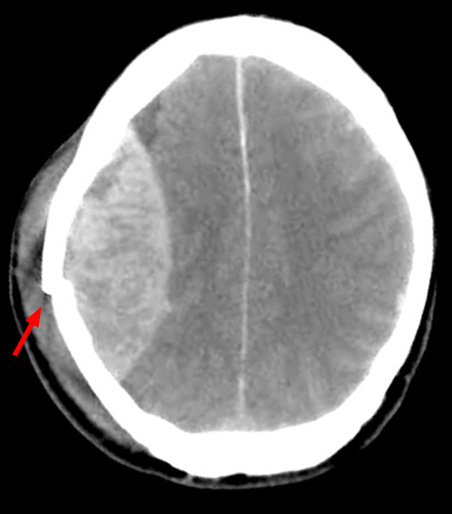
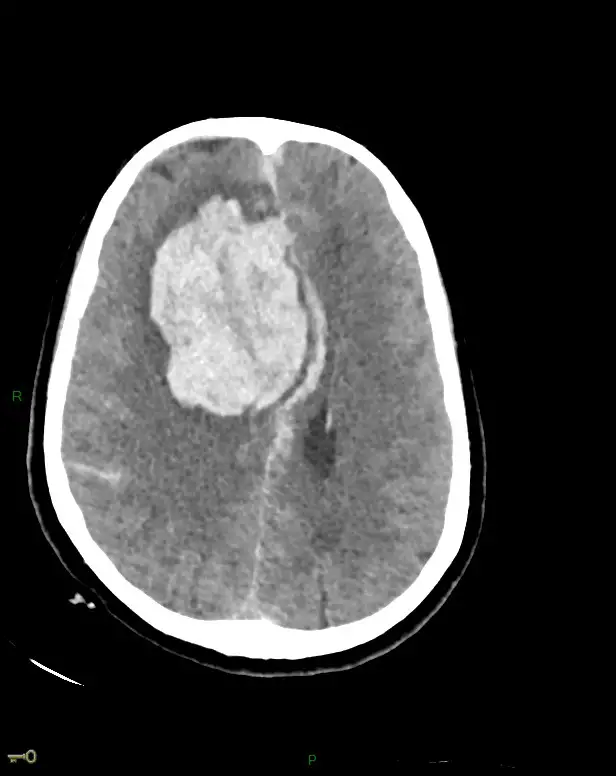
CT scan is the diagnostic test of choice forsubdural hematoma. This examination is done without injection of contrast product. L'subdural hematoma appears as a white lesion (hyperdense) on the CT scan, attached to the skull bone, curved in shape (falciform), with poorly defined contours. This collection of blood respects half of the brain and therefore does not extend to the entire circumference of the skull. The vertical membrane separating the two hemispheres of the brain called the false cerebri prevents this extension.
In any case, the scanner appreciates the importance, the volume and the mass effect of thesubdural hematoma on the other structures of the cranium.
Treatment of subdural hematoma
THEsubdural hematoma may be minimal causing few or no symptoms. In this case, therapeutic abstention is observed, since the blood often resorbs spontaneously in adults. However, strict clinical monitoring and scannographic monitoring must be done.
For large hematomas with apparent clinical symptoms, the neurosurgeon will drain the blood by performing a trepanation. This operation consists of piercing the cranial box with a circular hole to access the brain.
In some cases, when the blood is too thick and cannot be drained through a small hole, the neurosurgeon has to make a larger opening called craniotomy. He can then ligate the vessels responsible for the hemorrhage and clean the blood clots. A drain is placed during the operation for several days in order to remedy any recurrence of thesubdural hematoma.
Recovery after the operation
After surgery to drain a subdural hematoma, it is common for the patient to suffer from headaches and pain at the opening site of the skull. Painkillers will therefore be prescribed to relieve them.
During their post-operative convalescence, the patient can gradually resume the activities of daily living (getting up, eating alone, talking, etc.). This phase can last several weeks or even months and can be marked by disorders of the mood or memory.
A phase of rehabilitation by specialists (physiotherapist, speech therapist, ergonomist) will therefore be necessary to help him in this process.
Sequelae and prognosis
Generally, a chronic subdural hematoma, properly managed, leads to an improvement in the condition of patients. On the other hand, with regard to a acute subdural hematoma extended, the survival percentage is 50%. In all cases, patient monitoring is essential because of the risk of recurrence of up to 20%.
Conclusion
Subdural hematoma whether acute or chronic, is an effusion of blood into the space between the dura mater and the arachnoid.
In adults, the main cause of a subdural hematoma is head trauma caused by a road accident or a fall. shaken baby syndrome is the cause in infants. Risk factors are alcohol, age and anticoagulant drugs.
The symptoms are commonly those of theintracranial hypertension and scanner is the paraclinical examination allowing the diagnosis to be made.
The possible treatments are therapeutic abstention, surgical drainage, functional rehabilitation and more importantly monitoring.