Article reviewed and approved by Dr. Ibtissama Boukas, physician specializing in family medicine
Discectomy is a surgical technique sometimes used in the treatment of herniated discs that do not respond to conservative treatment (natural treatments and non-invasive methods).
What is a discectomy, and how do you know if you can benefit from it? How does the procedure take place ? What is the difference with other operations?
This article explains everything you need to know about this type of surgery.
Definition
Discectomy is a surgical technique that aims to "unblock" the nerve inside the spine by correcting a herniated disc problematic.
The herniated disc can be located anywhere, but mainly at the cervical level and at the lumbar level. We therefore distinguish:
- Lumbar discectomy
- Cervical discectomy.
Note: To know everything about herniated disc (diagnosis, symptoms, natural and invasive treatment approaches), see the following article.
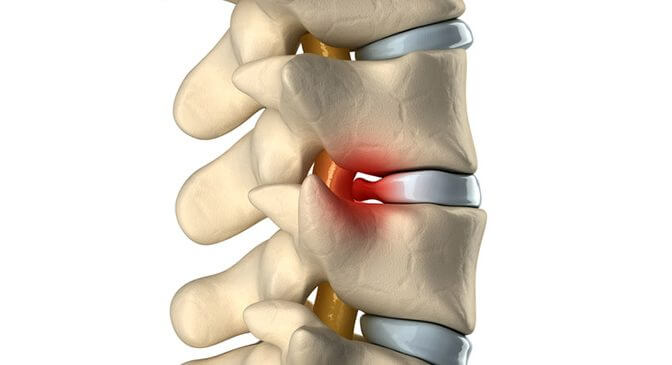
As a reminder ; The spine is made up of a succession of vertebrae. Between each vertebra there is a disc which acts as a shock absorber. We find two parts, the nucleus (in the center) and the annulus (which is the other part located peripherally).
The peripheral part serves as an envelope for the core. The annulus can be torn, frequently by wear, which leads to the compression of the nerve inside the vertebral column following the escape of a part of the nucleus; It's a herniated disc.
Hernias are often discovered incidentally; sometimes occurring following an effort, but sometimes without any favorable circumstance.
Other types of decompressive surgery
Alternatives to discectomy include:
- Laminectomy
- Laminoplasty
- Corpectomy
- Foraminotomy
- Arthrodesis
- Flavectomy
It should be noted that the optimal surgical technique to treat spinal or nerve root compression remains controversial. One approach is not necessarily superior in all circumstances, and the best option will depend on patient-specific anatomical and symptomatic factors.
Indications and contraindications
Indication for discectomy
The management of seizures sciatica acute improves 90% with conservative management. In rare cases, it may require surgery. Thus, discectomy is indicated in the following cases:
Emergency :
- If you have a cauda equina syndrome ;
- In case of a hyperalgesia sciatica resistant to morphine and other painkillers;
- Also in case of a sciatica paralyzing: a score of less than 3 on the health professional's muscle assessment for the muscles of the toes.
In case of persistent pain after 6 to 8 weeks of complete medical treatment when the pain remains disabling. The persistence of radiculalgia on lumbar pain is an essential criterion that leads to discectomy. Through these elements, the proposal of the discectomy is made to the patient by specifying the following elements:
- The natural progression of herniated discs and the risk of recurrence;
- In the event of non-possible medical treatment, surgery remains the last opportunity;
- Before the discectomy, the risks and benefits of the operation are assessed.
Contraindication of discectomy
Discectomy is not totally contraindicated. However, here are some factors to consider before deciding on a discectomy:
- For a lack of harmony of the clinical/radiological results (patient whose clinical results do not coincide with the radiological results.
- Patients with permanent back pain (Patients with mainly back pain without DNA radiation to the legs are not good candidates for discectomy)
- The patients who benefit the most from surgery are those who mainly suffer from radicular pain (sciatica).
- Inadequate conservative treatment: the patient must undergo a trial of adequate conservative management (at least 6 weeks of physical therapy such as physio, osteo, etc.) before surgery, because 90% of cases of sciatica improve with conservative treatment alone.
Discectomy procedure
Before a lumbar or cervical discectomy; the clinical and radiological assessment is preponderant in the precision of the approach and the technique to be used. (Chest X-ray, electrocardiogram, hematological analysis).
In addition, the patient must stop the consumption of tobacco, alcohol, blood-thinning drugs and anti-inflammatories seven days before the operation.
The discectomy takes place in several phases:
Phase 1: Pre-incision assessment is required
Phase 2: Incision and exposure of the intertransverse space
Phase 3: Opening of the intertransverse fascia and exposure of the hernia
Phase 4: Root release and excision of the hernia. The excision of the herniated disc is not always easy as the compression can be important. The ablation is done preferentially on the shoulder of the root.
Phase 5: closure and postoperative
Risks and complications
Like any surgery, there are risks and complications for discectomy. Thus we will distinguish the following risks:
Neurological risks
This is the risk of paralysis of the lower limbs. It can be a simple paralysis of the toes but sometimes more annoying with an attack on the level of the foot or the knee.
Difficulty urinating may occur and may require catheterization. It almost always regresses.
Very rarely there may be a cauda equina syndrome (paralysis of the sphincters, and even more exceptionally complete paralysis of the lower limbs (paraplegia).
The most common complication is hematoma at the site of the operation which can lead to compression of the nerves.
The infectious risk
Several types of infection are possible at the level of the bone and the disc producing spondylodiscitis; it can leave sequelae such as low back pain.
In some cases the infection can become generalized and lead to sepsis which can be very serious or even fatal.
Other risks
- A lesion of the great vessels of the abdomen (aorta, vena cava) occurring during excision of the disc. It can lead to severe bleeding that can be fatal.
- Recurrence: there is a risk of recurrence after a free interval. This is then another disc fragment which also comes into contact with the nerve.
Recovery from discectomy
Post-operative instructions
Like any surgical intervention, every 2 days a nurse does The dressing of the operative wound until healing.
In general, the sutures resorb during the 15 days following the discectomy; If the sutures are not resorbable, they must be removed by the nurse beyond 15 days.
Standing and sitting are authorized from the very day of the intervention in the company of the medical team to ensure that it takes place correctly.
Instructions on the economic gestures of the back are given; An analgesic treatment is systematically given the first days of the operation.
It can sometimes be done in outpatient surgery; The surgeon is seen again for a follow-up consultation 6 weeks after the intervention.
How long does the hospitalization last?
- Hospitalization lasts from 1 to a few days depending on the case.
- Depending on the nature of the professional activity, the localization of the hernia, the severity and duration of the symptoms, the duration of the work stoppage will be 3 to 12 weeks.
- Walking is recommended upon return home. It is possible to resume a sports activity after rehabilitation and a delay of 3 to 6 months depending on the type of sport and the speed of recovery.
Bibliography
SOFCOT: French Society of Orthopedic Surgery & Traumatology, practical advice, herniated disc, September 2005.
Dr Sébastien LE PAPE, Laminectomy and lumbar recalibration Estuary Private Hospital
B. FEY et all, treatise on surgical techniques, volume I, Masson, 1942-1944, P248-249
A.BLAMOUTIER, Surgical discectomy for lumbar disc herniation: surgical techniques, Elsevier Masson, 2012, 216-225
Medscape, Lumbar discectomy
SFCR: French Society of Spine Surgery, Intervention for lumbar disc herniation, November 2006