Do you suffer from sharp and intermittent lower limb pain that is ruining your life? If the answer is yes, it is likely that your symptoms are due to a sciatica.
But if your leg pain is accompanied by low back pain (lower back pain), you are rather dealing with a lumbosciatica.
Thanks to this article, you will know precisely what a lumbosciatica and know its symptoms, causes and different treatments.
Lumbosciatica: some notions of anatomy
Our spine (or spine) is made up of 5 parts, from top to bottom:
- Cervical part,
- Dorsal (or thoracic) part,
- Lumbar part,
- Sacral part (the sacrum),
- Coccygeal part (the coccyx).
La lumbar spine, or " Lumbar spine ", is composed of 5 voluminous vertebrae superimposed and separated from each other by discs intervertebral, of fibrocartilaginous structures which act as shock absorbers by absorbing the various shocks suffered by the spine.
Each of the lumbar vertebrae is made up of a bulky part in front called « vertebral body » and a thin rear part called " spinal blade » ou "posterior arch".
The vertebral body and the posterior arch of each vertebra delimit a space called "vertebral foramen". The superposition of all the foramens of the spinal column forms a bony tunnel inside which travels the spinal cord : the Spinal canal. This is divided into three parts:
- Le cervical canal containing the cervical cord whose nerve roots give rise in particular to the brachial plexus intended for the innervation of the upper limb,
- Le dorsal canal containing the dorsal cord giving rise, among others, to the intercostal nerves.
- Le lumbar canal containing the lumbar spinal cord which participates in the formation of the lumbosacral plexus.
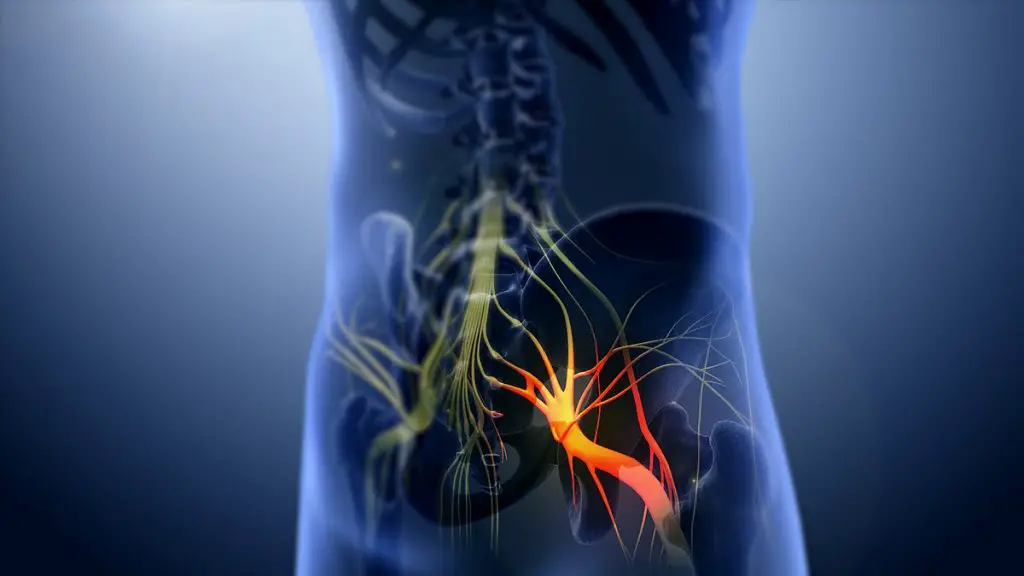
Le lumbosacral plexus, from the lumbar and sacral nerve roots (L4 to S3), gives rise to the largest nerve in our body: the nerf sciatica.
Le sciatic nerve ensures the motor and sensory innervation of the lower limb. It is precisely the compression (by one herniated disc for example) or irritation (inflammation) of this nerve which causes severe pain along its route (buttocks, thighs, knees, legs and feet).
This condition is called a « sciatica », and we will rather speak of "lumbosciatica" when lower back pain, or low back pain, is added to pain in the lower limb.
What is sciatica?
La lumbosciatica is therefore a pathology that combines two types of pain: those of the neuralgia sciatica (pain following the course of the sciatic nerve secondary to irritation of the latter) and low back pain (lower back pain).
Sciatica is generally due to a hernia discal lumbar, but other causes are possible such as spinal osteoarthritis, narrow lumbar canal and, much more rarely, certain serious pathologies (bone tumors).
Lumbosciatica Vs Sciatica: what's the difference?
La lumbosciatica is nothing but a sciatica to which are added lower back pain !
Sciatica, sciatica, lumbago, lumbosciatica, lumbosciatalgia… It is sometimes difficult to navigate with all these numerous scientific terms! But all it takes is a clear and concise explanation to understand the nuances:
- Sciatica: This is the term commonly used to designate the "sciatica neuralgia" which is pain following the path of the sciatic nerve following an irritation of the latter (compression by a herniated lumbar disc or inflammation for example).
- Sciatica: this term is composed of "sciatica" referring to the sciatic nerve, and "algia" which means pain. It is used to refer any pain in the area of the sciatic nerve, even if it is not due to irritation of the latter.
- Lower back pain: this term is used to designate any pain in the lower back (the lower back), regardless of its origin (spinal, renal, muscular, etc.).
- Lumbosciatica: it's a sciatica (or sciatic neuralgia) to which are added low back pain (lower back pain).
- Lumbosciatica: this term is used to designate any pain that involves the lumbar region and that of the sciatic nerve, regardless of its cause.
What are the causes of lumbosciatica?
There’s plenty of lumbosciatica say "communes" are the result of a disco-radicular impingement, that is to say a pathological interaction between a disk intervertebral and nerve root.
In 90% of cases, this disco-radicular impingement is secondary to a lumbar disc herniation, a protrusion of a lumbar intervertebral disc that compresses and irritates one of the nerve roots forming the sciatic nerve.
This pathology generally occurs for the first time on the occasion of a typical effort carrying a heavy load : excess stress on a probably worn lumbar intervertebral disc, the rupture of the peripheral layer of the latter, its pulpy nucleus is exteriorized through this rupture and presses on a nerve root.
There are other causes of sciatica:
- Lumbar osteoarthritis: osteoarthritis in the lumbar joints can be the cause of sciatica either by compressing one or more nerve roots by osteophytes (bony growths observed during osteoarthritis), or by irritating them by the diffusion of joint inflammation.
- Le narrow lumbar canal : narrowing of the lumbar canal (spinal stenosis) can manifest as lumbosciatica (low back pain and in the path of the sciatic nerve) in addition to other neurological symptoms such as sensory-motor disorders (tingling, loss of sensitivity, muscle weakness, intermittent claudication…).
- A benign or malignant vertebral tumour: a tumor process can compress a lumbar nerve root and trigger lumbosciatica.
- There’s nothing quite like a vertebral fracture : a displaced bone fragment or inadequate consolidation (bone repair after a fracture) can, in rare cases, cause lumbar nerve compression with sciatica.
- A bone infection: spondylodiscitis (infection of an intervertebral disc and vertebral bodies), epiduritis (infection in the epidural space), meningo-radiculitis, etc.
What are the symptoms of lumbosciatica?
Sciatica is characterized by two master symptoms: lower back pain (lumbago) and pain along the lower limb (following the course of the sciatic nerve).
In many cases, it is only "lumbar aches" who have settled in such a way insidious, without the patient being able to remember the exact circumstances of their appearance (sudden movement or “turn of the back”, carrying a heavy load, fall, etc.).
Indeed, repetitive strain injuries of everyday life can progressively damage and weaken the intervertebral discs, particularly those of Lumbar spine. This can cause, over time, progressive bulge one or more of these discs with the progressive compression one or more nerve roots.
Le painful repercussions is then, too, gradual and moderate. At this stage, it is possible to act on the risk factors to prevent a rapid evolution towards a severe herniated disc (weight loss, no carrying of heavy loads, etc.).
In other cases, low back pain appears from brutal way on the occasion of a trauma which the patient remembers precisely during his medical examination (fall, lifting a heavy load, etc.).
There’s plenty of low back pain et sciatica of the common lumbosciatica have characteristics that generally allow the diagnosis to be made fairly quickly (while awaiting confirmation by an imaging examination):
- They are exacerbated by cough, sneezing or any other movement that increases intra-abdominal pressure.
- They can be accompanied by sensory disorders in the lower limb such as tingling, tingling, sensations of electric shocks...
- They can be accompanied by motor disorders in the lower limb such as muscle weakness (paralysis in extreme cases).
- They are awakened or aggravated by the Lasègue maneuver (or test of SLR) : this is a maneuver that the doctor performs during the physical examination in order to clarify his diagnosis. It consists of stretching the sciatic nerve by raising the lower limb of the patient, keeping it straight (patient in a supine position). This sign is said " positive " when the movement triggers pain in the path of the sciatic nerve or when it is limited (the patient blocks his leg to avoid feeling the pain).
Sometimes the symptoms of lumbosciatica are more discreet ou interesting and unusual. Hence the need to consult a qualified healthcare professional to benefit from a complete clinical examination, any additional examinations and personalized care.
How is lumbosciatica diagnosed?
Diagnosis of sciatica is largely based on the interrogation et physical examination. Symptoms are usually strongly suggestive and the presence of a Lasègue sign leaves little room for doubt. A medical treatment will therefore be directly instituted with regular clinical monitoring to assess response to treatment.
In the vast majority of cases, when disc origin lumbosciatica seems very likely on clinical examination, no additional examination will be necessary whether the symptoms could be controlled by two to three weeks of medical treatment.
In case of resistance to well-conducted medical treatment for two to three weeks, a standard radiographic assessment will be taken with X-rays of the entire lumbar spine from the front and in profile in a standing position as well as X-rays centered on specific areas (particularly L5-S1).
This first-line assessment makes it possible to highlight certain signs of possible abnormalities favoring lumbosciatica, including lumbosacral hinge anomaly, narrow constitutional lumbar canal, spondylolisthesis by isthmic lysis, spondylosis or degenerative retrolisthesis, posterior osteoarthritis, etc.
When is it necessary to go further than the standard X-ray?
The doctor will prescribe a scanner or an Lumbar MRI in the following situations:
- Immediately in case of suspicion of lumbosciatica of infectious, tumoral or rheumatic origin. In other words, when it is not a common lumbosciatica (herniated disc). A blood test will also be carried out in search of certain biological markers (tumor markers, inflammatory syndrome, infectious syndrome, etc.).
- Immediately in case ofurgency surgical such as paralyzing lumbosciatica and cauda equina syndrome. These complicated forms require management as soon as possible, preferably within a surgical unit specializing in spinal pathologies.
- After six to eight weeks in case of symptoms not resolving with proper medical treatment during this period.
Lumbosciatica: MRI or scanner, which imaging test is the most effective?
In France, the realization of a first-line lumbar CT scan is still justified in the great majority of cases of common lumbosciatica. This imaging test has been proven to be as powerful as MRI for the diagnosis of a disco-radicular impingement secondary to a herniated disc.
The scanner is also the most effective examination for detecting within a herniated disc calcifications whose presence contraindicates the realization of a chemonucleolysis, a process that aims to destroy the hernia chemically (using a substance called chymopapain).
However, MRI is preferred to CT in the following situations:
- In case obesity: because fatty tissue alters the quality of the images, especially between L4-L5 and L5-S1.
- If you have a major scoliosis, for a better study of the vertebral foramina with sagittal sections.
- If you have a narrow lumbar canal
It also happens that the doctor prescribes an MRI after having requested a scanner in first intention if the latter did not reveal any anomalies despite the presence of symptoms (or not explaining them). An MRI will then be performed to look for a rarer cause such as a tumor (not detectable during the scan performed), a discrete disco-vertebral infectious process, etc.
It is important to remember that, in the vast majority of cases, no imaging is necessary for common sciatica. It is generally a benign pathology that can be treated in a few days/weeks with measures simple therapies (analgesic drugs, muscle relaxants, lifestyle, avoid carrying heavy loads, etc.).
What is the treatement lumbosciatica?
The management of sciatica depends on its cause. He can be radical (surgical) ou preservative (medical).
Only a doctor is able to develop an adequate therapeutic strategy after taking into consideration all the parameters, in particular:
- Age of the patient, his general state of health, Its antecedents medical and surgical...
- La severity of symptoms and their resounding on the patient's quality of life.
- La cause of lumbosciatica: is it a herniated disc or a tumour/infectious process…
- The presence or absence of complications (paralyzing lumbosciatica, cauda equina syndrome, etc.).
- Le patient's choice: the doctor always involves his patient in the therapeutic decision-making after having fully informed him of the advantages and disadvantages/risks of the various options.
In the following section, we will present the different therapeutic strategies common lumbosciatica (linked to a herniated disc):
Drug treatments
There’s plenty of simple analgesics such as paracetamol, nonsteroidal anti-inflammatory drugs and/or weak opioids (based on codeine, caffeine, tramadol, etc.) represent the first-line treatment in front of uncomplicated acute lumbosciatica.
This treatment can be started as soon as the diagnosis is made. common lumbosciatica, without the need for confirmation by imaging. It is usually enough to relieve symptoms in just a few days.
Other drugs, such as muscle relaxants (muscle relaxants) or certain antiepileptic (pregabalin), may also be prescribed to better manage pain with a strong muscular or neuropathic component.
After a few days of drug treatment, the doctor re-evaluates his patient in order to detect a possible complication (having settled secondarily) oradapt the treatment if necessary.
Attention, although most of the drugs used in first intention in common lumbosciatica are over the counter, it is not recommended to use them without the supervision of a qualified health professional.
physiotherapy sessions
La physiotherapy represents one of the pillars of the management of uncomplicated common sciatica. Many techniques can be used by the physiotherapist to provide symptom relief, including:
- The massages: to reduce muscle tension that causes pain.
- Lumbar traction: it consists in reducing, thanks to precise and controlled maneuvers, the stress exerted on the lumbar intervertebral discs in order to decompress the nerve root(s) and obtain temporary relief.
- La McKenzie method : it consists in identifying the movements and postures at the origin of pain in order to be able to correct them and obtain relief.
- therapeutic exercises aimed at relieving symptoms and improving function.
Local corticosteroid injections
In case of'failure of well-conducted first-line drug treatment for at least 6 weeks (analgesics, physiotherapy, general measures), the doctor may suggest corticosteroid injections directly at the level of the pathological areas to reduce the inflammation there, and therefore the pain.
Corticosteroid infiltrations relieve pain associated with lumbosciatica on an ad hoc basis, maximum three times a year. This is a temporary measure, the effects of which are not necessarily immediate, which is generally used during painful flare-ups.
In the event of failure of corticosteroid injections, contraindications or patient refusal, stronger pain medications may be offered by the doctor (especially morphine).
The surgical intervention
Apart from emergencies, the surgery should only be considered in last resort, that is to say after all conservative treatments have failed mentioned above (analgesic drugs, corticosteroid injections, physiotherapy, etc.).
In some cases, surgery should be considered immediately:
- Lumbosciatica complicated by paralysis (paralytic lumbosciatica).
- Lumbosciatica complicated by cauda equina syndrome (urinary incontinence, loss of sensitivity in the buttocks, bladder, etc.).
- Lumbosciatica hyperalgesic, that is to say with pain deemed unbearable by the patient and resistant to the most powerful painkillers (morphine, oxycodone).
- Lumbosciatica whose symptoms persistent beyond 4 to 8 weeks or gradually getting worse despite proper medical treatment.
The various surgical procedures aim to decompress the nerve root(s), in particular the cure of a hernia, the removal of a bone fragment, the correction of a vertebral slippage, etc.
Resources
Reference
[1] E. Masson, “Common lumbosciatica”, EM-Consult. https://www.em-consulte.com/article/271161/lombosciatique-commune (accessed August 30, 2022).
[2] R. Thurel, “Lombosciatica by herniated disc”, Acta neurochir, flight. 2, no 1, p. 9‑31, March 1951, doi: 10.1007/BF01406095.
[3] “Recommendations Common acute lumbosciatica”, VIDAL. https://www.vidal.fr/ Maladies/recommandations/lombosciatique-aigue-commune-3527.html (accessed September 12, 2022).
[4] L. Bellaïche and É. Enkaoua, "Choice of imaging in common lumbosciatica", Review of Rheumatism, flight. 71, p. S77-S84, August 2004, doi: 10.1016/S1169-8330(04)80008-5.
[5] E. Legrand, T. Couchouron, P. Insalaco, and M. Audran, “Should a patient suffering from common lumbosciatica be hospitalized? », Review of Rheumatism, flight. 71, p. S100-S103, August 2004, doi: 10.1016/S1169-8330(04)80013-9.
[6] “Corticoid infiltrations in sciatica and common low back pain – ScienceDirect”. https://www.sciencedirect.com/science/article/abs/pii/S1169833008001014 (accessed September 16, 2022).
My name is Katia, I am specialized web editor in writing medical articles. Being passionate about medicine and writing, I set myself the goal of making medical information accessible to as many people as possible, through the popularization of even more complex scientific concepts.