Are you 50 or older, suffer from osteoarthritis and complain of lower back pain? You have to think of a sciatica or to a herniated disc. What if it was a degenerative spondylolisthesis ? Or at least have you ever heard of it?
It is simply a slip progression of vertebrae linked to aging of the spine. Is that bad ? What is the link with osteoarthritis? Is it a curable disease? I invite you to read this article, you will find all the answers to these questions.
What is degenerative spondylolisthesis?
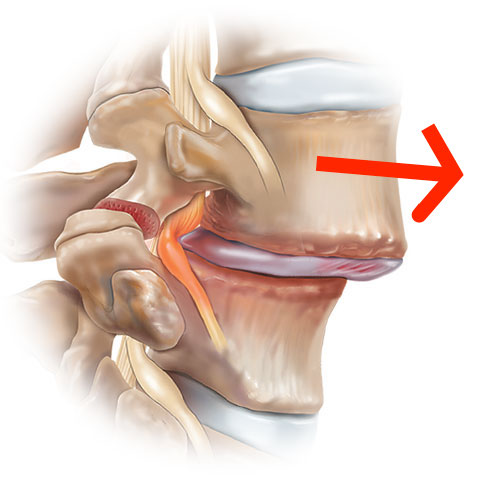
Le spondylolisthesis is a Latin term meaning “slippage of the vertebrae”. This phenomenon occurs when one vertebra slides over another vertebra just below, protruding forward from the alignment of the spine (vertebral column).
Le degenerative spondylolisthesis, as its name suggests, is the consequence of a progressive degeneration of the bone structure of the spine of osteoarthritic origin. It most often affects the vertebrae L4 / L5 being the most mobile and therefore the most fragile part of the spine.
Affected subjects are generally fifties and sixties with a female predominance. In addition to lower back pain, these subjects may report radicular pain (sciatica, cruralgia) related to the compression of the nerve roots as a result of slippage.
Nevertheless, there are two other types of spondylolisthesis with different origins and characteristics:
- Le spondylolisthesis by isthmic lysis: the mechanism of this type of sliding is linked to a spondylolysis or fracture of the isthmus or of the segment serving as a bridge between two vertebrae. The fracture is said to be of fatigue and most often results from the repetition of the stresses suffered by the spine.
- Le dysplastic lumbar spondylolisthesis: It is about a congenital malformation characterized by an abnormal elongation of the isthmus of the last vertebra. Generally, this anomaly does not require any particular management apart from clinical and radiological monitoring.
To learn more about the various types of spondylolisthesis, see the following article.
What causes degenerative spondylolisthesis?
As mentioned in the definition, degenerative spondylolisthesis is of origin osteoarthritis. This means that the physiological aging of the patient but also all the risk factors for osteoarthritis are incriminated in the occurrence of this pathology.
The risk factors for osteoarthritis and therefore for degenerative spondylolisthesis are, among others:
- Regular carrying of heavy and substantial loads,
- The genetic factor: it is certain that osteoarthritis is not a genetic disease, but a person with a family history of osteoarthritis may be genetically predisposed to have this pathology
- Le overweight : the link between obesity and osteoarthritis seems well established. The greater the weight, the lower the strength of the frame.
- La menopause et theosteoporosis
Diagnosis of degenerative spondylolisthesis
Medical imaging is essential to document spondylolisthesis. Sometimes, the symptoms of the latter are quite suggestive, and the history combined with the clinical examination can suggest a diagnosis of spondylolisthesis.
The interrogation will bring us the notion of low back pain or sciatica. The clinical examination will direct us towards the presence or not of a lumbar stiffness and signs of nerve compression in advanced forms.
Once the diagnosis of spondylolisthesis has been evoked, the X-ray of the Lumbar spine standard is the first-line radiological examination to be performed. Thanks to the face, profile and oblique incidences, we can visualize the vertebral bodies and isthmuses and highlight the sliding between two vertebrae.
La standard radiology also makes it possible to quantify slippage by estimating the degree of advancement of one vertebra relative to the other and therefore classify spondylolisthesis into grades (Meyerdig classification or Taillard index).
In the case where the clinical examination reveals neurological signs such as paresthesias or motor deficit, the doctor will have to complete the radiological assessment with a CT (scanner) or a MRI of the lumbar spine. This will allow him to better visualize the slippage and look for a possible narrowing of the lumbar canal.
How to recognize degenerative spondylolisthesis?
Low back pain et sciatica are the classic clinical interpretation of degenerative spondylolisthesis.
The diagnosis of degenerative spondylolisthesis should be considered in an adult over the age of 50 who complains of lower back pain of varying intensity.
These pains can be located in the lumbar region, more precisely at the L4-L5 level and remain well tolerated for a long time. Sometimes, they can be acute and appear suddenly on the occasion of a triggering factor such as carrying a heavy load.
A sciatica is frequently found in patients, who define it as pain starting in the lower back and radiating to the buttocks or down both legs and feet. This means that the slip caused irritation of the sciatic nerve.
In the advanced forms, the compression of the nerve roots can be irreversible and lead to more or less serious consequences, such as:
- Le tail syndrome cheval : whose name comes from the appearance of the nerve roots emerging from the spinal cord. Being responsible for the innervation of the organs of the pelvis and lower limbs, their compression will cause sensory-motor disorders and sphincter disorders (impotence, urinary incontinence, constipation…).
- A paralysis members: which can be partial or complete.
Other symptoms can be observed inconstantly such as: paresthesias, a intermittent claudication, tingling or numbness in the lower limbs.
How to treat spondylolisthesis?
The therapeutic management of spondylolisthesis is based on two types of treatment.
- Conservative treatment : Medication and functional rehabilitation
- Invasive treatment : infiltration or surgery
Medical treatment
In first intention, the doctor prescribes analgesics and non-steroidal anti-inflammatory drugs. The doses and routes of administration will depend on the intensity of the pain. He will therefore opt for the molecules of level I: paracetamol, NSAIDs, aspirine.
If the pain is intense and throbbing from the outset, we can prescribe weak opioids of stage II (codeine, dextropropoxyphene, tramadol), or strong opioids (morphine).
Personalized lumbar infiltrations are also prescribed, especially in the case of radicular pain or pain resistant to oral treatment.
Functional rehabilitation
Rehabilitation is an essential complementary approach that includes specific exercises to relieve pain and improve the quality of your life.
After a thorough assessment of your case, a set of specific exercises will be offered to you by your physiotherapist (physiotherapist). The program may include, among others: pelvic tilt exercises, abdominal strengthening; the double knee to the chest; activation of the stabilizing muscles of the spine (multifid, spinal erectors, iliocostal, etc.).
When to operate?
Surgery occurs when medical treatment alone or combined with rehabilitation has not led to the expected results. What is the case of 10 to 20% patients with spondylolisthesis. However, in the event of spondylolisthesis complicated by motor neurological disorders (paralysis) or sphincter disorders, surgery may be required immediately.
Technically, it involves correcting the slippage between two vertebrae by carrying out a vertebral arthrodesis or consolidated fusion of two vertebrae. This intervention is carried out using osteosynthesis (screws and rods) which are placed via the posterior approach.
The aim of the operation is to remove the nerve compression and therefore to relieve the disabling pain associated with spondylolisthesis.
My name is Anas Boukas and I am a physiotherapist. My mission ? Helping people who are suffering before their pain worsens and becomes chronic. I am also of the opinion that an educated patient greatly increases their chances of recovery. This is why I created Healthforall Group, a network of medical sites, in association with several health professionals.
My journey:
Bachelor's and Master's degrees at the University of Montreal , Physiotherapist for CBI Health,
Physiotherapist for The International Physiotherapy Center