The spinal infiltrations corticosteroids are routinely used in the treatment of many pain root canals et neuralgia cervico-brachial. Their primary objective is to suppress any inflammation involved in the genesis of pain, and therefore to relieve or even eliminate the latter.
THEcervical infiltration may be effective in the treatment of certain chronic neck pain. However, its analgesic effect is of short duration, even sometimes absent… It is therefore important to know the indications and the dangers of this procedure; a precise assessment of the risk-benefit ratio is required before resorting to it.
What is cervical infiltration?
In the medical field, theinfiltration refers to the injection of a liquid substance (containing an active ingredient) directly into the area to be treated, outside the blood vessels. This method is used in particular in anesthesia (injection of an anesthetic substance near a nerve to block nerve impulses), and in rheumatology with the injection of anti-inflammatories (corticosteroids) in certain joints.
L'cervical infiltration is therefore a medical procedure that consists of injecting an active ingredient, usually corticosteroids (anti-inflammatories), directly at the source of neck pain. Thus, the drug acts locally by reducing inflammation and pain sensations without diffusing to the whole body as when receiving an intravenous injection or an oral treatment (general or systemic route).
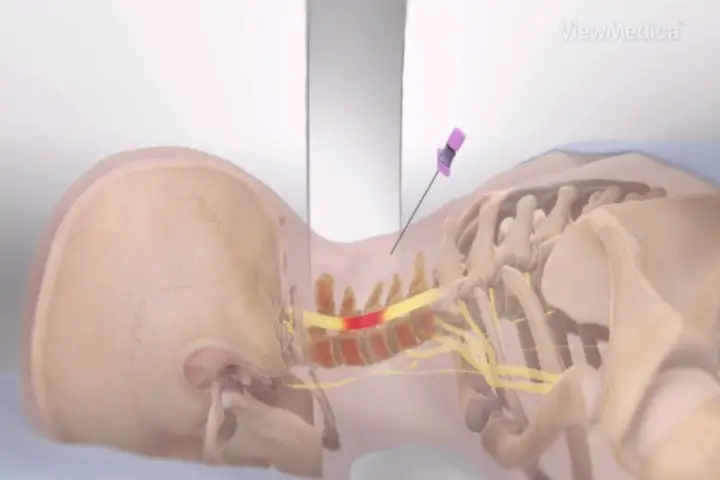
The cervical infiltration is done at the level of the epidural fatty space of the spinal canal (between the bone and the dura mater, the outermost envelope of the central nervous system). For example, this makes it possible to reduce the inflammatory phenomena at the level of a nerve root compressed by a cervical disc herniation, and thus relieve pain.
What are the indications for cervical infiltration?
Cervical infiltration is considered in certain chronic neck pain in the event of failure of the various first-line drug treatments (analgesics, anti-inflammatories, physiotherapy, etc.).
It is offered in the radiculalgia of the upper limb in connection with a conflict between the intervertebral disc and a cervical nerve root. Often as part of a herniated disc.
According to the latest recommendations, neck pain should persist for more than 7 weeks despite well-conducted medical treatment before considering cervical infiltration.
Obviously, there must not be a significant neurological deficit, as this would require different management (surgery).
In certain situations, cervical infiltration may be considered even if the pain has lasted for less than 7 months, particularly in the case of neck pain hyperalgesic of root origin (very intense pain resistant to morphine).
What are the contraindications of cervical infiltration?
Cervical spinal infiltration is contraindicated in the following situations:
- Hemodynamic instability: we do not perform cervical infiltration in a patient with acute heart failure, for example…
- Platelet dysfunction syndrome: a condition characterized by an inability of platelets to aggregate to form a platelet plug. There is therefore a hemorrhagic risk in the event of the procedure being carried out.
- Severe thrombocytopenia: insufficient number of platelets. The risk here too is the occurrence of bleeding that is difficult to control.
- Bleeding disorder: hemophilia, Von Willebrand disease, taking anticoagulant treatment.
- History of trauma cervical.
- Intercurrent infection (fever, chills…).
- Sepsis (presence of bacteria in the blood).
- Local infection: at the injection site.
There are also relative contraindications, that is, it is possible to perform cervical infiltration despite their presence (provided that they are corrected or the patient is closely monitored). Among them, we can cite theallergy to contrast medium and taking treatment antiplatelet platelet (aspirin, clopidogrel, etc.).
What are the risks of cervical infiltration?
Cervical infiltration, despite being widely used in the treatment of root pain, is not without risks and complications.
Infectious risk
As with any invasive procedure, there is a risk infectious. In fact, despite rigorous aseptic measures, infection is always possible at the injection site. The latter can subsequently spread to neighboring structures or cause sepsis (presence of bacteria in the blood).
Fortunately, these infections are relatively rare (1-2%) and are usually minor.
However, more serious infections have been reported:
- Epidural abscesses.
- Meningitis.
- Osteomyelitis (bone infection).
- Septic arthritis (joint infection).
- Spondylodiscitis (infection of vertebral bodies and intervertebral discs).
Bleeding risk
The epidural space is a richly vascularized structure. Thus, during a cervical infiltration, there is a possibility of injuring a blood vessel, which can result in a spinal hematoma (i.e. pooling of blood) in the cervical region.
The hemorrhagic risk is obviously higher in patients with a hemostasis anomaly or a coagulation disorder (hemophilia, current anticoagulant treatment, etc.).
Allergic risk
There is a risk of réactions allergic ou anaphylactic contrast product, anesthetic product or corticosteroids. They can appear within two hours of the injection, but they are quite rare.
Detailed questioning, close monitoring of hemodynamic parameters and a trained team ready to intervene if necessary are always necessary when performing this procedure.
Risk of neurological complication
Surveys of radiologists have identified a worrying number spinal cord infarction which occur as a result of cervical spinal infiltrations.
Other neurological complications related to this procedure have been reported:
- Vascular accidents: that can affect the brain (CVA), spinal cord or the cerebellum.
- Epidural hematomas (accumulation of blood in the epidural space).
- Spinal cord injury.
- Infarction medullary ou central by embolism.
- convulsions (rare).
- Pneumencephaly (presence of air in the cranial box following a breach).
- Blindness (temporary or long-lasting due to retinal necrosis or chorioretinopathy).
- tetraplegia with risk of death from cardiac arrest.
How is a cervical infiltration performed?
When you suffer from neck pain chronic, several drug treatments can be offered to you depending on the pathology that causes them. Only if these treatments fail will your attending physician consider other alternatives such as cervical infiltration, or even surgery as a last resort.
Once the cervical infiltration is proposed, you will go through different stages.
First, you will be referred to an operator radiologist for a specialized consultation. The latter will question you, examine you and consult your medical file (containing the various examinations carried out: x-rays, scanners, MRI, biological assessment, etc.) in order to, among other things:
- Make sure that there is indeed an indication to perform the gesture.
- Check the absence of contraindications (infection, coagulation disorder, etc.).
- Identify the precise site of the conflict and its nature (possibly by carrying out a new scanner).
Then, once all these checks have been made, you will be explained the different stages of the procedure that you will undergo as well as its risks and side effects. If you are taking antiplatelet treatments, you will be asked, in agreement with your doctor or cardiologist, to stop them at least 5 days before the procedure.
Finally, you will be called for the realization of the cervical infiltration. This procedure is performed in an x-ray office. It only lasts about twenty minutes and includes the following steps:
- Installation on the scanner table: your radiologist or one of his team members will place you on the scanner table in a prone position. Indeed, cervical infiltration is performed with CT guidance to very precisely reach the pathological site while avoiding damage to the various neighboring structures.
- Identification of the site to infiltrate: the target of the infiltration is identified precisely and in real time thanks to the scanner.
- Preparing the injection site: the skin area is carefully disinfected then anesthetized locally. The entire procedure will be carried out with the greatest respect for aseptic measures in order to reduce the risk of infection as much as possible.
- Introduction of the needle : up to the site to be treated (posterior joint, etc.), always under CT guidance.
- Injection of the contrast product : the radiologist injects a small quantity of iodine (contrast product) which will confirm the correct position of the needle and avoid damaging the various organs.
- Injection of corticosteroids : once the needle is in the right position, we inject corticosteroids (infiltration itself).
- Needle removal : once the infiltration has been performed, the needle is carefully withdrawn by the radiologist, still under CT guidance. A dressing will be applied to prevent the risk of infection.4
During the infiltration, you may feel pain similar to what you usually feel (reproduction of pain).
Once the procedure is complete, you will be asked to stay for around XNUMX minutes under observation to ensure that there are no abnormal signs. You can then go home with the matters made cervical infiltration and your medical records.
Cervical infiltration: Aftermath
After performing a cervical infiltration, a resurgence of neck pain can be felt during the first two days. Do not worry, just take a painkiller and rest, they usually give in 24 to 48 hours. A work stopping may be prescribed to you by your GP.
The response to cervical infiltration varies from one patient to another and depending on the indication, the nature of the lesions... The reduction in pain is noticeable 3 7 days in after the gesture on average.
However, the result is not always there. It is sometimes necessary to reschedule a second session of cervical infiltration (usually after a month). The maximum number of cervical infiltrations that can be performed is 3 per year.
In case of non-response to cervical infiltrations, the patient is referred to surgery for a specialist consultation (as a last resort).
References
[1] P. Brunner et al., “Percutaneous infiltrations of cervical, thoracic, and lumbar spine”, in Seminars in interventional radiology, 2002, vol. 19o 03, p. 219-228.
[2] E. Masson, “Cervical and lumbar foraminal infiltrations under scanner”, EM-Consult. https://www.em-consulte.com/article/751576/les-infiltrations-foraminales-cervicales-et-lombai (accessed March 17, 2022).
[3] Evangelia Passia and Stéphane Genevay, “Complications of spinal infiltrations”, Swiss Medical Review. https://www.revmed.ch/revue-medicale-suisse/2017/revue-medicale-suisse-553/complications-des-infiltrations-rachidiennes (accessed March 16, 2022).
[4] C. Cyteval et al., “Cervical radiculopathy: open study on percutaneous periradicular foraminal steroid infiltration performed under CT control in 30 patients”, Am. J. Neuroradiol., flight. 25, no 3, p. 441-445, 2004.
My name is Katia, I am specialized web editor in writing medical articles. Being passionate about medicine and writing, I set myself the goal of making medical information accessible to as many people as possible, through the popularization of even more complex scientific concepts.