Disc disease T11-T12 (also called D11-D12) is caused by disc damage between the last 2 vertebrae of the thoracic region. It can cause various symptoms depending on each individual, and the main cause of the problem.
Its management must absolutely take into account the dysfunctions associated with this condition, as well as the general condition of the patient.
This article covers everything you need to know about T11-T12 disc disease.
Definition and anatomy
Before talking about T11-T12 disc disease, it is worth discussing the anatomy of the vertebrae dorsal and lumbar to better understand this condition.
The dorsal vertebrae (or dorsal spine) are 12 in number (numbered D1 to D12). The alignment of these vertebrae means that they allow a lot of rotation.
The lumbar vertebrae (or Lumbar spine), they are 5 in number. Unlike the dorsal column, these vertebrae are not very mobile in rotation. Rather, their alignment allows for more movement in flexion and extension.
The junction between the last vertebrate dorsal and first vertebrate lumbar is called thoraco-lumbar hingee (also called D12-L1). This site is under a lot of stress because it is a transition zone between the end of the dorsal vertebrae and the ribs with the lumbar vertebrae.
In addition, there are several nerves that emerge from the thoracolumbar junction. Damage to these nerves will cause pain depending on their distribution.
For example, affected nerve roots innervate including the lower lumbar region, upper buttocks, sacrum, groin, labia majora or scrotum, trochanteric region (hip), and outer thigh .
Causes
Among the potential causes of T11-T12 disc disease are the following conditions:
Dorsal hernia
A herniated disc occurs when the fibers of the fibrous annulus surrounding the disc are cracked, and the gelatinous core migrates to the periphery. The distorted disc can therefore irritate surrounding structures (spinal cord, spinal nerves, nerve roots, ligaments, etc.) and cause symptoms.
In the dorsal region, there is very little space around the spinal cord. So, a herniated disc at this level can be more serious than hernias located at the cervical or lumbar level. In some cases, a back hernia can even cause weakness in the muscles below the waist, even leading to paralysis.
Fortunately, herniated discs in the thoracic region are not as common as in the lumbar spine.
To learn more, see this article on dorsal hernia.
Maigne syndrome
Any dysfunction of the thoraco-lumbar junction leads in particular to pain that radiates to the lower back and its surroundings. It can be joint or disc damage (such as a back hernia), or nervous. This condition is referred to as Maigne syndrome, or the syndrome of thoraco-lumbar hinge. This condition was named after French orthopedic physician Robert Maigne.
To learn more about Maigne syndrome, click here.
Facet arthritis (zygapophyseal)
Zygapophyseal osteoarthritis is an osteoarthritis that affects the posterior inter-apophyseal joints of the spine, also called zygapophyseal joints. It mainly affects the cervical and lumbar vertebrae, but can also affect the thoracic vertebrae.
Osteoarthritis can indirectly cause a reduction in the space between the T11 and T12 vertebrae, thus causing discopathy at this level by wear of the T11-T12 disc.
To learn more about this condition, check out this page.
Back osteoarthritis
Although the dorsal column is less likely to degenerate in comparison with the cervical or lumbar regions, it is not immune to degenerative and osteoarthritic phenomena. Whether it is the general wear and tear of the spinal joints over time (normal aging), or certain predisposing factors, it is possible to develop back osteoarthritis.
Here are some potential causes favoring the appearance of this disease:
- heavy lifting
- history of falls
- trauma
- road accident
- Scoliosis or scoliotic attitude
- infection
- genetic factors
- etc.
To know everything about back osteoarthritis, see the following article.
Symptoms of the disease
People with symptomatic T11-T12 discoapthia may experience the following symptoms:
- Dorsolumbar pain (between the lower thoracic and upper lumbar region)
- Radiation of pain to the rib cage or trunk
- Localized swelling, redness and tenderness
- Muscle spasms
- Difficulty leaning back, standing, and walking
- Difficulty sitting still for long periods
- Morning stiffness
In some cases, dorsal disc disease will compress important structures (such as the spinal cord) and lead to potentially serious consequences. This constitutes a medical and sometimes surgical emergency. Therefore, it is essential to consult without delay if you observe any of the following signs:
- Tingling, numbness and/or weakness in the arms, hands, legs or feet.
- Lack of coordination and difficulty walking
- Loss of sensation in the perineum area
- Uncontrollable muscle spasms
- Loss of sphincter control (urinary and fecal incontinence)
- Constant pain not relieved by rest
- Chest pain or severe abdominal
To find out about all the situations where back pain is the result of a serious injury, see the following article.
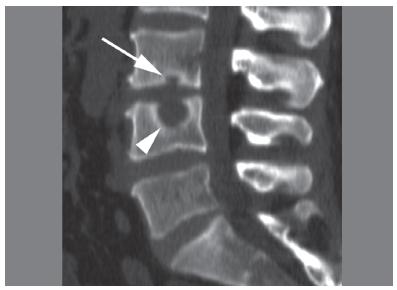
Diagnostic
T11-T12 disc disease is confirmed by medical imaging. An X-ray is sufficient to see the reduction in space between the vertebrae, although the doctor may order a CT scan or magnetic resonance imaging (MRI) to clarify the diagnosis.
It should be noted that the presence of discopathy at the dorsal level is not necessarily synonymous with pain or pathology. Indeed, there are many asymptomatic cases, i.e. people who present with degenerative changes to themedical imaging without showing any symptoms. This comes from the ability of the human body to adapt despite the presence of dorsal discopathy. Often, it is said that the pain will appear if there is nerve irritation, or if an inflammatory phenomenon is triggered.
To determine the functional consequences of back osteoarthritis, a health professional will perform a clinical examination to better define the diagnosis. This will include an assessment of trunk movements, reflexes, sensitivity, muscle strength, etc. These elements will make it possible in particular to exclude serious breaches of the spine, and guide the treatment plan.
Treatment
Here are some treatment options often used in the treatment of T11-T12 disc disease:
Medication
As with low back pain, anti-inflammatories, pain relievers and/or muscle relaxants are prescribed to calm the inflammation and pain.
heat and ice
Heat and/or ice are often used to relieve back pain symptoms.
These modalities should be applied at the thoraco-lumbar level to obtain significant relief (although it is often temporary).
For the difference between heat and ice, see next article.
Myofascial release and massage
As the thoraco-lumbar region is often hypersensitive and hypertonic, muscle relaxation techniques can relieve symptoms.
For example, massage techniques, palpation-rolling, and myofascial release can be used by a therapist. Obviously, he will adapt his approach according to the patient (superficial vs deep techniques).
Joint mobilization and manipulation
In the presence of T11-T12 discopathy, it is possible that the thoracolumbar region is hypomobile. This means that the D12 and L1 vertebrae do not move enough in the sagittal plane.
Although these findings are subjective, manual work by a therapist (such as an osteopath) to mobilize the vertebrae may be beneficial in reducing pain and other symptoms.
Spinal traction techniques are regularly used to reduce stress on the thoracolumbar junction. This will also reduce the pressure on the nerves emerging from this site, which are sometimes irritated. In addition, spinal manipulations at the lower dorsal level may also be relevant in certain cases.
Eventually, manual work from an osteopath could act on the sympathetic and parasympathetic systems to relieve symptoms. Although the mechanism of action of osteopathic manipulations is controversial from a scientific point of view, they generally offer good clinical results.
Postural correction
Without wanting to blame poor posture as the cause of T11-T12 disc disease, you should know that prolonged static postures can cause back pain.
So tips and exercises to straighten your back may help relieve symptoms in some cases, and prevent future pain.
In certain specific cases, the use of a posture corrector may be helpful in preventing trunk sagging. On the other hand, these devices fix the body in a precise position, and can inhibit the action of the postural muscles in the long term.
To know the opinion of a physiotherapist on the posture correctors (and when to use them), see the following article.
Exercices
In general, passive manual techniques (that is, administered by a therapist) offer short-term results only. It is for this reason that an active approach is always recommended as a complement.
Exercises aimed at opening up the thoraco-lumbar space can be prescribed by a physiotherapist, for example. They often involve bending and sideways tilting movements aimed at reducing stress on the affected side.
When the pain is under control, trunk stabilization exercises should be done to prevent recurrences. This involves strengthening the back, lumbar, peri-scapular (around the shoulder blades) muscles, etc.
If the patient wants to return to sport, it will be necessary to analyze the movements and requirements specific to the sport practiced. Then, a gradual return will be considered, with rehabilitation focused on optimizing sporting gestures.
Infiltration
A treatment option when symptoms do not subside is infiltration.
To learn all about back infiltration (and the different types), see the following article.
What about natural remedies?
Although they are not supported by solid scientific evidence, several natural products and home remedies are used to treat back pain, especially for their anti-inflammatory power. It is essential to consult a doctor beforehand, mainly to avoid drug interactions and side effects.
Here is a non-exhaustive list of plants and essential oils that are effective in controlling pain and inflammation. The products are available on the site Country. Use promo code LOMBAFIT15 if you wish to obtain one of the following products, or any remedy aimed at relieving your symptoms and improving your quality of life:
- Turmeric. Thanks to its antioxidant and anti-inflammatory powers very powerful, turmeric is one of the most used plants in a culinary and therapeutic context. The composition of turmeric is essentially made of essential oils, vitamins (B1, B2, B6, C, E, K) and trace elements. But it is to its composition rich in curcumin and curcuminoids that we owe them and calm skin of this spice.
- Ginger. In addition to the special flavor it brings to the kitchen and its aphrodisiac properties, ginger is a root well known for its anti-inflammatory powers. the gingerol gives it its anti-inflammatory action. It is an active component acting on the inflammatory pain related to chronic joint inflammatory diseases, including rheumatoid arthritis, lupus, rheumatic diseases, etc. It has been proven that this active element is also effective in acting on the inflammation linked to arthritis and sciatica. Ginger also has other benefits thanks to its high potassium content and its richness in trace elements (calcium, magnesium, phosphorus, sodium) and vitamins (provitamin and vitamin B9).
- Omega-3s. Omega-3s are polyunsaturated fatty acids that play a very important role in the functioning of our body. They are provided by food in three natural forms: docosahexaenoic acid (DHA), alpha linolenic acid (ALA) and eicosapentaenoic acid (EPA). Beyond their action on the brain and the cardiovascular system, omega-3s prove very effective against inflammation. Indeed, they have the ability to act on the inflammatory mechanisms in osteoarthritis by slowing down cartilage destruction, thus they reduce the intensity of osteoarthritis pain. There sciatica, being most often related to an inflammation secondary to a herniated disc, it can also respond to omega-3 provided it is consumed regularly.
- Lemon eucalyptus. Eucalyptus is a plant most often used in the form of herbal tea or essential oil. She would have anti-inflammatory effects which give it the ability to act on the bone and joint pain in general and the pain of sciatica in particular.
- wintergreen. Wintergreen is a shrub from which a very interesting essential oil is extracted. It is one of the most used essential oils in aromatherapy. This oil extracted from the shrub bearing the same name, is used in massage to relieve sciatica and act like a analgesic. Indeed, it provides a heating effect thanks to its ability toactivate blood circulation locally.
Remember that these products do not replace medical treatment. Do not hesitate to consult for support adapted to your condition.