The temporomandibular joint is one of the most stressed joints in daily life. It is useful to us especially for food and for speaking. Due to these many functions, this joint is exposed to multiple pathologies that can cause discomfort and pain when opening the mouth. And in this article we are going to talk about thetemporomandibular osteoarthritis. Discover the causes and the different ways to manage this joint pathology.
Definition and anatomy
What is temporomandibular osteoarthritis?
THEOsteoarthritis temporomandibular corresponds to a osteoarthritis of the jaw joint. It reflects the degradation of all joint structures (cartilage, bone and meniscus).
jaw joint anatomy
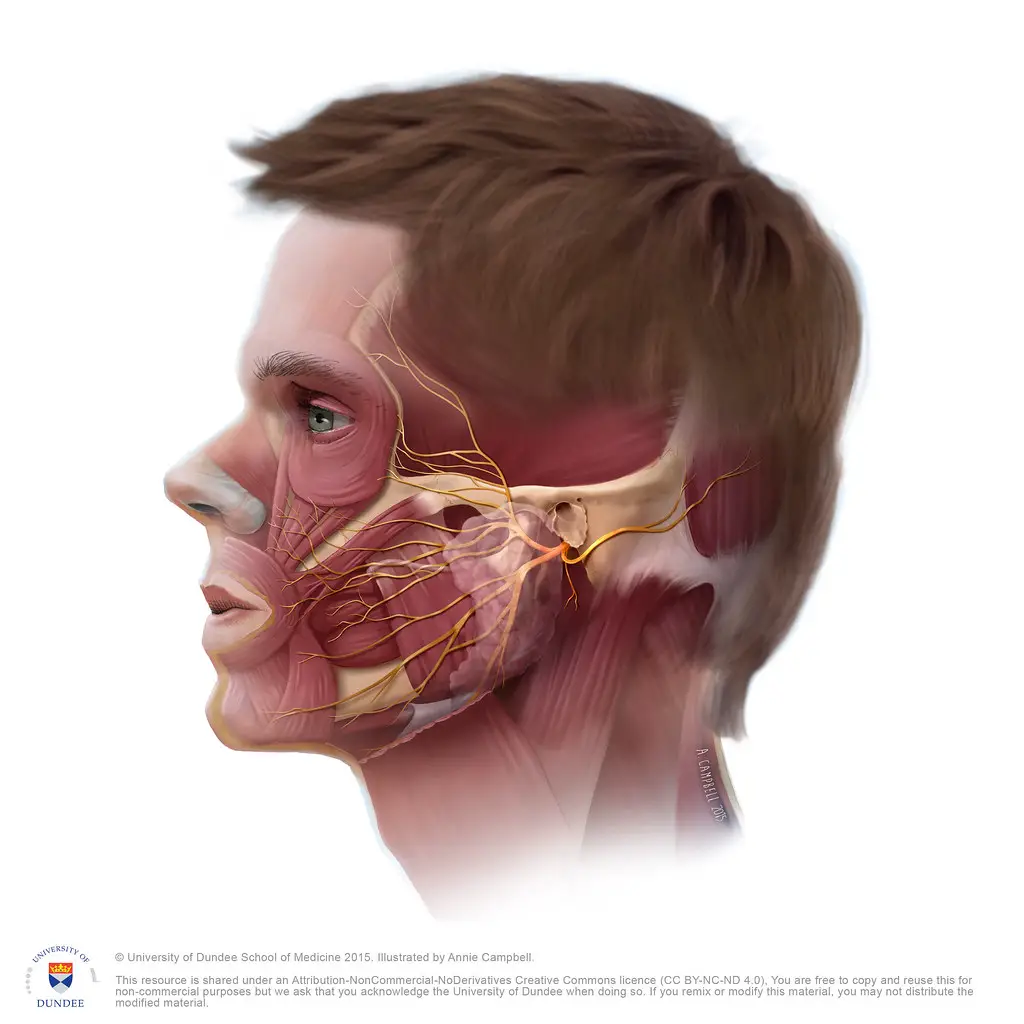
THEjoint temporomandibular also known by the abbreviated term ATM is the joint that connects the upper jaw and the mandible.
It is a diarthrosis (or synovial) joint of the bi-condylar type. She is extremely mobile. It is held together by ligaments, tendons and muscles.
Like all synovial joints, ATM lodges inside a joint capsule. It unites the mandibular fossa of the temporal bone with the condyle of the mandible (jaw) through an articular disc formed of fiber and cartilage.
There are two TMJs located in both sides of the face, in front of each ear. These two joints always work in sync, and perform two types of movement.
- The opening of the mouth which is carried out by a rotation of the condyle of the mandible with the articular disc.
- The lateralization of the jaw which occurs when there is translation between the articular disc and the temporal bone.
They thus allow the movements of the mandible in relation to the skull and offer several functions:
- salivary or prandial (food) swallowing;
- chewing;
- phonation;
- the yawn.
What is the difference between osteoarthritis and temporomandibular arthritis?
It is true that temporomandibular osteoarthritis and temporomandibular arthritis are very similar. They both affect ATM. The manifestations are very similar, because as with osteoarthritis, arthritis also manifests itself by inflammation of the joint area and by pain and limitation of movement of the jaw. However, it is not the same pathology.
THEOsteoarthritis temporomandibular is a mechanical, degenerative joint disease characterized by wear and tear on all structures of the jaw joint. Osteoarthritis in general refers to the disease of the cartilage. On the contrary, thearthritis temporomandibular encompasses all inflammations at the ATM level.
Temporomandibular arthritis includes inflammation of the tissues located on the ATM generally caused by the presence of foreign microorganisms in this part.
The origin of arthritis is often unknown, but in most cases it comes from an autoimmune reaction. In this self-defense mechanism, the human body attacks its own tissues and leads to arthritis in general.
There are several types of temporomandibular arthritis depending on the origin.
The only way to tell temporomandibular osteoarthritis apart from temporomandibular arthritis is by X-ray imaging.
Probable causes of the development of temporomandibular arthrosis
The causes of temporomandibular osteoarthritis can be many. The most important are those that lead to wear and tear of the cartilage. The articular cartilage deteriorates leading to inflammation of the TMJ.
In TMJ osteoarthritis, the fibrous disc and bone structure undergo remodeling and change shape. These are called degenerative changes. Once the disc shifts or perforates, symptoms of osteoarthritis appear.
There are also other causes of temporomandibular osteoarthritis:
- abnormalities of the dental articulation;
- facial trauma and fractures;
- stress and prolonged anxiety;
- parafunctions: unconscious hyperactivity or bob of the jaw often associated with grinding during sleep and dental wear;
- hyperlaxity due to the presence of ligaments that are too loose or too relaxed;
- a rheumatic disease...
Characteristic symptoms of temporomandibular osteoarthritis
The main signs that indicate the presence of osteoarthritis of the jaw concern both the mechanism, the pain and the functioning of the ATM.
For mechanical signs, the most characteristic are crackles or crackles when opening the mouth (cracking jaw), difficulty in chewing, limitation of the opening of the mouth as well as blockages or recurrent dislocation of the jaw.
As for the pain, it manifests itself especially during the opening and closing of the jaw. The patient may experience temple pain, sinus pain, headache, migraines, feeling of pressure or otitis in the ears, facial neuralgia, neck pain or shoulder pain… Some people also feel burning on the tongue during this joint disease.
In TMJ osteoarthritis, the patient also has difficulty chewing and is sometimes confronted with hearing problems. We mainly talk about tinnitus (an erroneous sensation of noise in the ear).
Diagnosis of temporomandibular osteoarthritis
The diagnosis of this pathology must be made with a doctor or a dentist. The procedure always begins with a palpation examination of the TMJ as the patient opens and closes their mouth. The practitioner thus observes any abnormal movements, pathological noises, inflammatory or painful reactions, etc. It should be noted that he must at the same time check for any other possible causes arising from other ENT or dental problems.
In case of perceptible cracking during the opening of the mouth, the diagnosis is oriented towards temporomandibular osteoarthritis. To confirm this, the doctor usually uses an X-ray.
Depending on the doctor's opinion, additional examinations such as CT scan, cone-beam type 3D digital radiography or MRI may be necessary. They are used to detect the presence of other pathologies that may be responsible for temporomandibular disorders such as:
- Costen syndrome
- Rheumatic disease
- Other jaw pain
Treatment of temporomandibular osteoarthritis
Treatment with analgesics, anti-inflammatories and sometimes muscle relaxants can relieve the symptoms of temporomandibular osteoarthritis. In case of failure, it is possible to make intra-articular injections based on betamethasone (AIS) and sodium hyaluronate. Intra-articular corticosteroid injections generally promise great effectiveness in reducing joint pain.
Botulinum toxin, in addition, also seems to be effective in the treatment of pain. Injected directly into the masticatory muscles (masseters and/or temporal and/or pterygoid), it helps them to relax which calms muscle and joint pain.
Functional TMJ treatment is also necessary to restore optimal dental occlusion. There are two main possibilities.
- Orthodontic treatment (grinding of teeth…).
- Wearing an occlusal device to stop pain and contractures. This is a relatively smooth bite plate over where the teeth rest, to allow them and the jaw to move unrestricted at rest.
Surgery is needed when there is a blockage in the opening of the mouth. Also, we must consider the prosthetic rehabilitation of posterior edentulism (loss of posterior teeth), frequently associated with temporomandibular osteoarthritis.
Physical therapy (physiotherapy) is also indicated to optimize the mechanics of the temporomandibular joint, strengthen the muscles involved in the stabilization and dynamics of the jaw, and to improve function.