La paralyzing cruralgia represents a fortunately rare complication of the common cruralgia but can sometimes occur and have a significant functional impact.
But what is its particularity? How does it manifest? And what is his treatment? Answers in this article.
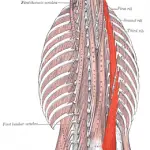
Lumbar Spine and Crural Nerve: Anatomy
La lumbar spine ou Lumbar spine designates the lower portion of the vertebral column, it is located under the dorsal part and is articulated by its last vertebra (L5) to the sacrum.
It is composed of five lumbar vertebrae (L1 to L5) articulating between them thanks to the articular surfaces which are dedicated to them and to ligaments.
Between each vertebra there is a fibrocartilaginous structure called intervertebral disc, the latter is formed of a part located in the center which is called " pulpy nucleus ", it is not innervated and very hydrated, and of a peripheral part, " fibrous ring “, which can be the seat of cracks with age.
The lumbar spine, when viewed laterally, is shaped like a " S ". This is the natural curvature of the lumbar spine called " lordosis ».
The main roles of the lumbar spine are the participation in the support of the head, the preservation of the posture of the trunk, the maintenance of the upright position, the mobility and finally the protection of the spinal cord and other nervous structures.
La spinal cord is located at the level of the spinal canal, it ends at the level of the L2 vertebra. Nerve roots originating from the spinal cord leave the vertebral column passing through orifices called " foramina ».
One of the nerves emerging from the lumbar spine is the femoral nerve also called crural nerve. It results from the union of anterior branches of three nerve roots: L2, L3, L4 at the height of the psoas major muscle. It is a motor muscle allowing the contraction of the muscles of the hip and the knee, but also sensitive because it ensures the sensitivity at the level of the anterior part of the thigh and the anterior and internal face of the rest of the lower limb.
What is cruralgia?
La cruralgia designates a monoradiculargia, that is to say a painful syndrome involving a single nerve root, of vertebral origin resulting in localized pain along the territory of the crural nerve.
She is met in 70% cases in humans, therefore predominantly male, regardless of their age but the age group of the 45 to 60 year-olds is usually the most affected.
Its onset is usually brutal and it readily occurs following a triggering incident such as a lifting effort, trauma to the lumbar region or even a hacking cough.
It is a pain, most often, very intense called " nagging “, readily occurring at night and worsening following an effort of coughing, defecation, walking or a sudden movement.
Like the sciatic nerve, the crural nerve is one of the most voluminous nerves in the human body. As a result, the pain concerning him can sometimes be very difficult to relieve.
As with sciatica, the topography of the pain depends on the affected nerve root. Although in half of the cases, the pain stops at the level of the knee, we nevertheless distinguish:
- Type L3 cruralgia: it starts at the level of the supero-external part of the buttock, goes around the hip, crosses the anterior face of the thigh up to its middle third then passes obliquely below and inside the thigh to finish at the inner side of the knee.
- Type L4 cruralgia: in this case, the pain also begins at the level of the buttock, it descends along the external face of the thigh to the lower third or it passes to the anterior face, it crosses the knee forward, the antero-internal face of the leg to end at the level of the internal edge of the foot sometimes up to the big toe.
Paralyzing cruralgia, what particularity?
Cruralgia is due to compression and irritation of one of the roots forming the crural nerve. This compression is the consequence of damage affecting the lumbar spine and may be of origin:
- degenerative like herniated disc,vertebral osteoarthritis, spondylolisthesis or narrow lumbar canal.
- infectious such as spondylodiscitis due to tuberculosis.
- tumor.
It is manifested, in addition to pain, by a hypoaesthesia (decreased sensitivity), feelings of tingling, electric shocks ornumbness at the level of the painful path, a abolition of the reflex patellar and in the most extreme cases, a cauda equina syndrome with sphincter disorders.
La paralyzing cruralgia is, as its name suggests, a cruralgia whose motor deficit reaches the stage of paralysis.
Paralyzing cruralgia is a real neurosurgical emergency. Indeed, the functional prognosis and the evolution of the deficit are dependent on the speed of management, but it happens that unfortunately, despite rapid and optimal management, the motor deficit persists or even worsens.
How to establish the diagnosis of paralyzing cruralgia?
Paralyzing cruralgia is clinically manifested by a motor deficit less than or equal to 3 at muscle testing whether of sudden or gradual installation.
The role of the crural nerve is to ensure:
- The flexion of the thigh on the trunk;
- Leg and knee extension;
- And incidentally, the abduction of the thigh.
Crural nerve palsy will therefore manifest itself by:
- An impossible flexion of the thigh;
- The inability to extend the leg;
- Abolished ankle reflex;
- Atrophy of the muscles of the anterior compartment of the thigh;
The impairment can be unilateral and accompanied by pseudo-stepping when walking, or bilateral, in which case walking will be impossible.
The diagnosis of paralyzing cruralgia is made clinically thanks to a examination and to a physical examination.
Its confirmation may require the performance of imaging tests such as:
- The scanner ou Lumbosacral CT: it allows to confirm the existence of a herniated disc and to determine the seat and the type by or to detect other causes of compression.
- THEMRI of the lumbosacral spine : it confirms the existence of a disco-radicular conflict (herniated disc), or of a compression due to another etiology such as a tumor or a tumoral cause.
What treatment for paralyzing cruralgia?
Paralytic cruralgia is considered a true neurosurgical emergency. It represents indeed with the cauda equina syndrome and hyperalgesic cruralgia absolute surgical indications and must imperatively be operated within 24 hours.
Surgical treatment consists of freeing the affected nerve root using different techniques such as chemonucleolysis, discectomy (Intergovernmental Panel on Climate Change) and the arthrodesis.
It should be noted that sometimes, despite successful surgery performed on time, some paralyzing cruralgia persists.
A post operative rehabilitation is essential to ensure good functional recovery and to avoid a recurrence of pain.
My name is Sidali. I am a general practitioner and Web Editor. As a healthcare professional, my mission is to contribute to the relief of my patients' ailments. Being also passionate about writing, I have the pleasure of sharing my solid medical knowledge with the greatest number of readers, by writing popular articles that are very pleasant to read.