La camptocormia, or " Bent Spine Syndrome (BSS), is a posture disorder, often misunderstood, which affects the elderly.
What is camptocormia?
The etymology of the term "camptocormia" comes from ancient Greek: “kamptos” which means « lean, and "cormos" designating trunk. It was first used in 1915 to refer to bowing of the trunk secondary to spinal trauma.
Camptocormia, also called “Bent Spine Syndrome” or even “progressive lumbar kyphosis”, is not a disease in itself, but a symptom ou clinical sign of an underlying condition.
It's about a involuntary anterior flexion of the trunk, accompanied by a hypolordosis lumbar, even a lumbar kyphosis at an advanced stage.
Definition of terms:
- Hypolordosis: decrease in lumbar curvature, but it remains concave (hollow).
- Lumbar kyphosis: inversion of the lumbar curvature. It becomes convex, instead of being concave in the normal state.
To know more about the difference between kyphosis and lordosis, see the following article.
Camptocormia occurs to the effort ou in standing up position. It is wholly or in large part reducible in a prone position or voluntarily through righting efforts. This particularity makes it possible to distinguish between spinal deformities of osteoarticular origin which are not reducible even in the supine position.
What causes camptocormia?
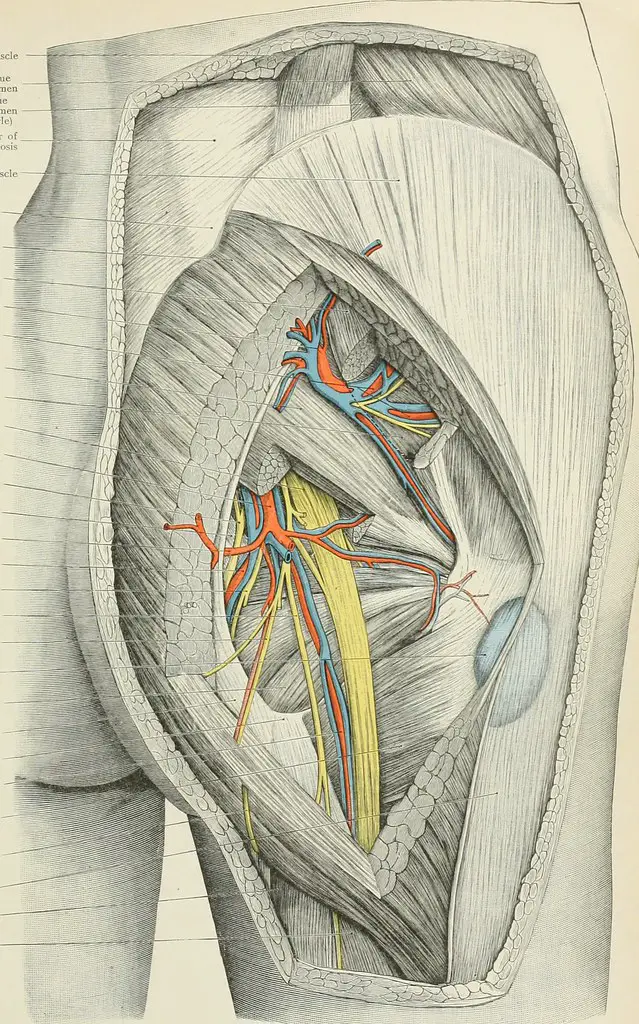
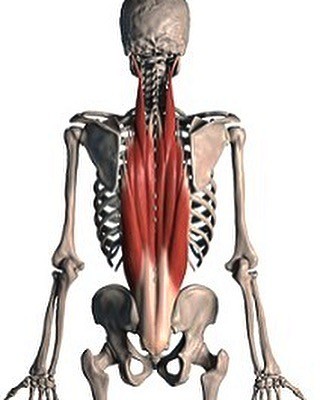
La camptocormia is consecutive to a deficit of spinal musculature, mainly in the lumbar region. The affected muscles are expanders innervated by the posterior branch of the spinal nerve. Their dysfunction can be of muscular or neurological origin.
The causes behind the dysfunction of these extensor spinal muscles are many and generally entangled. We can cite :
- Origin muscular: dystrophic, myotonic, inflammatory myopathies, etc. The muscles affected are often the erector spinae muscles, multifid, iliocostals, etc.
- Origin neurological : many neurological conditions can include in their clinical picture the symptom of camptocormia. Examples include amyotrophic lateral sclerosis (ALS or Charcot's disease), Parkinson's disease, narrow lumbar canal, cerebrovascular accident (CVA), post-poliomyelitis syndrome, polyneuropathy chronic inflammatory demyelinating disorder with involvement of the posterior branch of the spinal nerve innervating the spinal extensor muscles…
- Iatrogenic origin: camptocormia can be the complication of a surgical procedure, in particular within the framework of a surgery of the spine (a laminectomies for narrow lumbar canal for example) with impairment of the spinal nerve responsible for the innervation of the extensor paravertebral muscles.
- Paraneoplastic origin: some cancers may be accompanied by camptocormia.
- General diseasess: such as hypothyroidism or osteomalacia.
- Psychiatric origin: camptocormia can be part of a hysterical crisis. In general, it is the female subjects who are concerned.
In most of the cases, no cause is identified. We are then dealing with a primary axial myopathy ou idiopathic. Some authors call it “late onset spinal extensor myopathy” (MTES), or late onset paravertebral myopathy.
There are frequent family forms of camptocormia (several members of the same family affected). The predisposition genetic is therefore probably one of the risk factors for this postural disorder.
Clinical features of camptocormia
This is how you recognize a person with camptocormia :
- It leans forward when standing or walking.
- She tries to maintain her balance on the sagittal plane (to avoid falling forward) by compensating for the trunk extension deficit by an extension of the hip, a semi-flexion of the knees and a support with the hands on the thighs.
- She brings her head back making a hyperextension of the neck when it is about to fall forward.
- The curvature of the trunk disappears when lying down.
- At an advanced stage, it may develop orthopedic disorders such as a dorsal kyphosis and/or irreducible lumbar, flexion of the knees, flexed hips.
Flessum: or flexum, it is the loss of mobility of a joint, its stiffness and its blocking in a more or less bent position.
How is camptocormia diagnosed?
Le diagnosis of camptocormia is largely based on the history and clinical examination of the patient. The clinical characteristics of camptocormia make it relatively easy to confirm its existence, especially in the advanced stages.
After confirming that it is indeed a camptocormia, and not of an osteoarticular disorder or other differential diagnosis, the rest of the diagnostic process will consist of determine its etiology (the causative disease).
To do this, the doctor may prescribe several Additional tests :
- Biology report : a blood sample is taken to look for biological markers of certain conditions (blood formula, inflammatory markers, thyroid and parathyroid function, autoimmune antibodies, etc.).
- Standard X-ray: it may prove useful in seeking an etiology for camptocormia. The standard X-ray of the vertebral column in front and in profile can highlight signs of osteoarticular involvement excluding the diagnosis of camptocormia such as a vertebral compaction, osteoporosis, signs in favor of ankylosing spondylitis… Moreover, it makes it possible to objectify lumbar hypolordosis and confirm the reducible character of the curvature of the trunk by taking images in the supine position.
- IRM ou computed tomography (scanner): these imaging examinations make it possible to study the paravertebral muscles in more detail. They can sometimes highlight signs of myopathy with fatty infiltration of the extensor paravertebral muscles.
- Electroneuromyography: this examination makes it possible to eliminate damage to the neuromuscular junction (zone of communication between a muscle and the nerve that controls it) or other nerve damage such as root compression in the context of a narrow lumbar canal.
- Muscle biopsy: it is sometimes necessary at the level of the extensor paravertebral muscles to highlight any histological changes (fatty infiltration of the muscle).
What are the treatments for camptocormia?
At the end of the clinical and paraclinical investigations, one can find oneself in one of the following two situations:
- Is an underlying disease is found (which is quite rare). The treatment of camptocormia then consists of specifically treat this underlying disease (surgery if narrow lumbar canal, synthetic hormone treatment if hypothyroidism, Levodopa if Parkinson's disease, etc.).
- Is no cause is found (the biological assessment is normal, imaging and electroneuromyography only show non-specific signs, muscle biopsy only shows abnormal fatty infiltration, etc.). We are then dealing with a camptocormia idiopathic ou late paravertebral myopathy the processing of which is purely symptomatic (even palliative sometimes).
The management of camptocormia should be precocious et multidisciplinary to avoid its aggravation. Indeed, the treatments used aim only to stop, or at least slow down, the evolution of the deficit, because unfortunately, obtaining an improvement is rare in the case of idiopathic camptocormia.
Drug treatments
Currently there is no treatment having proven its effectiveness in slowing down the evolution of idiopathic camptocormias. Of the analgesics can be prescribed in case of associated back pain.
Re-education
The treatment of camptocormia is largely based on the physiotherapy (physiotherapy). The protocols are not clearly defined, but it is essential.
Au initial stage, physiotherapy sessions may include exercises:
- Strengthening the paravertebral muscles.
- Strengthening the muscles of the pelvic girdle and lower limbs.
- Cardio-respiratory kinesis (the deformation of the trunk compresses the lungs and the heart, which interferes with their functioning).
- Postural rehabilitation.
- Proprioceptive work (deep sensitivity).
- Muscle stretching.
Has a more advanced stage, once the paravertebral amyotrophy has progressed, the physiotherapy sessions will aim to limit retractions muscles, tendons, ligaments and capsular to reduce vicious attitudes. They also aim to relieve some pain through analgesic techniques and physiotherapy.
In addition to rehabilitation, it is essential for a patient with camptocormia to practice regular physical activity and to have a balanced diet in order to avoid weight gain which would greatly complicate his situation.
Corset
Un corset specially designed for correct trunk anteflexion and to regain (or preserve) the lumbar lordosis is prescribed to patients with camptocormia. It is generally advised to wear it at least 4 hours per day (spread over the day), although the duration of wearing varies from patient to patient.
Several other types of trunk expander corsets exist and can be used. The most important thing is to adapt them regularly according to the evolution of the anteflexion and the complaints of the patient.
surgery
The indications are not yet clearly defined and are studied on a case-by-case basis. Spine surgery can be considered in case of aggravation of camptocormia despite well-conducted conservative treatment (drugs, rehabilitation, lordosis corset, etc.).
One of the radical surgical modalities for camptocormia is to merge several vertebrae du Lumbar spine and dorsal (arthrodesis). This allows the spine to be straightened, at the cost of its immobilization…
To learn more about thelumbar arthrodesis, see the following article.
This option is reserved for motivated patients and in good general condition, as it is very heavy and involves long and difficult rehabilitation sessions, not to mention its many short and long-term complications.
Resources (videos)
Projects
[1] T. Stojkovic, “Camptocormia: diagnosis and treatment”, Neurological Practice – FMC, flight. 6, no 2, p. 71-79, March 2015, doi: 10.1016/j.praneu.2015.01.002.
[2] M. Hogge and A. Debrun, “Camptocormia: from diagnosis to treatment”, Rev Med Brux, p. 5, 2016.
[3] J. Finsterer and W. Strobl, “Presentation, etiology, diagnosis, and management of camptocormia”, European neurology, flight. 64, no 1, p. 1-8, 2010.
[4] K. Karbowski, “The old and the new camptocormia”, spine, flight. 24, no 14, p. 1494, 1999.
[5] M. Laroche, MB Delisle, R. Aziza, J. Lagarrigue, and B. Mazieres, “Is camptocormia a primary muscular disease? », spine, flight. 20, no 9, p. 1011-1016, 1995.
My name is Katia, I am specialized web editor in writing medical articles. Being passionate about medicine and writing, I set myself the goal of making medical information accessible to as many people as possible, through the popularization of even more complex scientific concepts.