Le bag dural is a kind of resistant sheath which contains our spinal cord. It protects this important nervous structure from various shocks.
In certain specific situations, the dural sac can be the seat of anomalies: dilation, narrowing et compression. Various symptoms may then appear, including motor, sensory and genito-sphincter disorders.
In this article we tell you more about the dural sac and its pathologies.
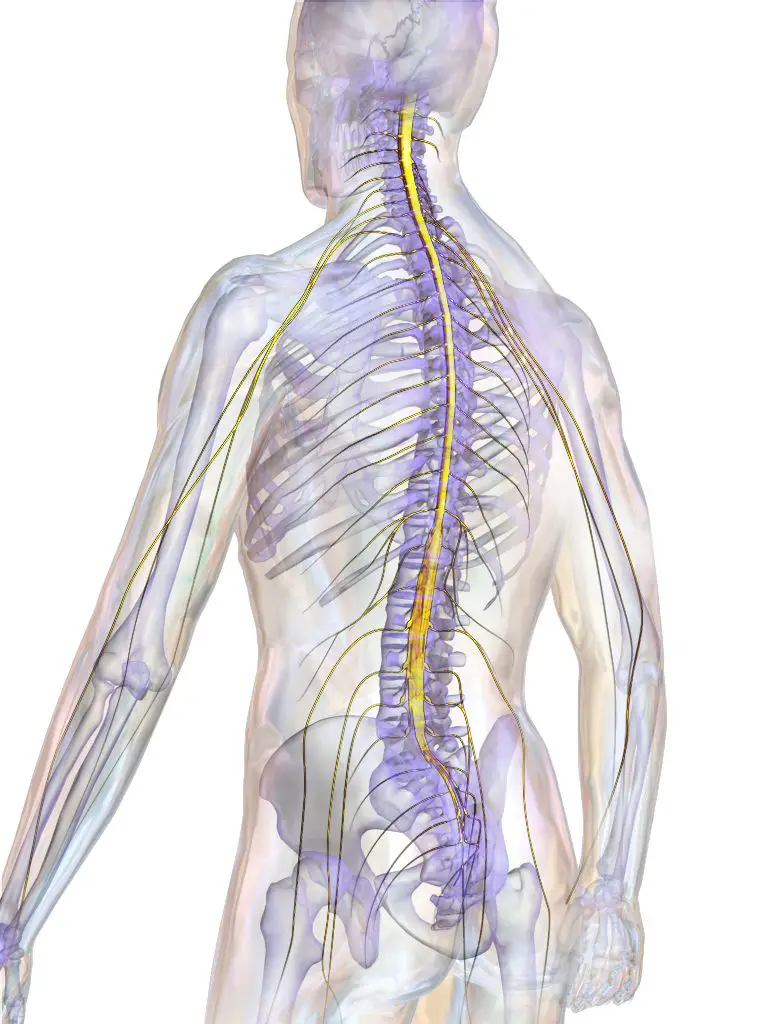
Spinal cord and dural sac: basic notions
La bone marrow spinal, or bone marrow spinal, is one of the major parts of our central nervous system (CNS). It originates at the level of the lower part of the brainstem and descends about 43 cm inside the Spinal canal. It ends between the first two vertebrae lumbar (L1 and L2) by a tapered part called "terminal cone".
The spinal cord provides many functions:
- Routing of nerve impulses from the brain to the muscles: moving, walking, etc.
- Transport of sensory information to the brain: sensation of pain, heat, etc.
- Coordination center for certain reflexes: for example, the ability to withdraw one's hand from a hot object very quickly, without even thinking (without the intervention of the brain).
- Physiological functions: urination, defecation, ejaculation…
The marrow is therefore a part very valuable of our organism. This is why it is protected by several elements (from the outside to the inside):
- The spinal canal: bony canal passing through the center of the vertebrae and containing the spinal cord,
- The dura mater: resistant fibrous membrane forming a protective sheath surrounding the entire CNS,
- THEarachnoid : under the dura mater. It is used, among other things, to fight against CNS infections,
- The subarachnoid space: in which the cerebrospinal (or cerebrospinal) fluid circulates.
- The pia mother: membrane attached directly to the spinal cord and the other elements of the CNS.
La tough mother therefore forms a kind of membrane sheath that contains and protects the spinal cord along its entire length. This structure is called the "dural bag" ou “thecal bag”.
Le bag dural extends from the base of the skull (around the foramen magnum, hole through which the spinal cord passes) to the second vertebrate sacred (S2) to cover the entire length of the spinal cord.
Inside this bag is the cerebrospinal fluid (CSF) in which bathes the spinal cord. This liquid is used, among other things, to protect the latter by absorbing the various shocks, to nourish it, to protect it from infections...
Throughout the spinal cord, the bag dural presents dural projections which follow the roots of the spinal nerves as they exit the spinal canal. They therefore form a kind of sheaths which protect these nervous elements.
Dural sac: pathologies and symptoms
Dural sac dilation
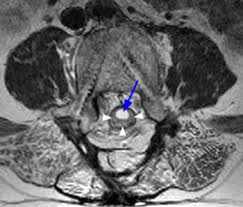
La dural sac dilation ou "mega cul-de-sac" is one of the late complications of ankylosing spondylitis (chronic inflammation of the joints of the pelvis and spine). It is characterized by an increase in the diameter of the dural sac in the lumbar or lower dorsal region.
To learn more about ankylosing spondylitis, see the following article.
The precise mechanisms behind this dilation are not well known. According to many authors, chronic inflammation of the joints of the spine would in turn induce inflammation in the subarachnoid space and the dura mater.
This would lead to a loss of epidural space and to a fibrous thickening of the dura mater. These two phenomena prevent the cerebrospinal fluid from circulating freely and being absorbed. He stagnates then at the level of bag dural and causes it to expand.
This dilation of the dural sac occurs gradually, after about thirty years of evolution of the disease (ankylosing spondylitis). It mainly affects men (84%).
Clinically, the dural sac dilation is manifested by the following symptoms (which settle insidiously):
- Sensory disorders (tingling, pain, decrease or loss of sensitivity in certain areas, in particular the perineal region and the lower limbs).
- Sphincter disorders (urinary incontinence, faecal incontinence, etc.).
- Genital disorders (impotence… Rare, but probably underestimated).
- motor disorders (fairly rare and usually minor).
Symptoms gradually worsen in the absence of adequate management. In the final stage, the patient is permanently bedridden (with all the complications of decubitus that entails) and totally dependent.
On the therapeutic side, there are not many possibilities:
- Drug treatments: inconsistent results.
- Surgical treatment, first option: represented by laminectomy (consists of removing part of one or more vertebrae in order to widen the lumbar canal and make more room for the dilated dural sac). Here too, the results are inconsistent (risk of infection or worsening of symptoms, etc.).
- Surgical treatment, second option: represented by the lumboperitoneal diversion. This technique consists of draining towards the peritoneum the cerebrospinal fluid which stagnates at the level of the dural sac thanks to a system of tubing and valves. The peritoneum is very effective in resorbing liquids, this property is also exploited in the treatment ofhydrocephalus (ventriculoperitoneal shunt).
Dural sac narrowing/compression
Le bag dural may be the seat of narrowing or compression in certain pathologies.
The dural sac is considered shrunken when its diameter is less than 10 mm, or when its area (in cross section) is less than 80 mm. Shrinkage is considered critical when these parameters become lower than 6mm and 50mm respectively.
La dural sac compression can have several origins. Most often, it is secondary to a degeneration osteoarthritis can be associated with a protrusion ou herniated disc.
In less than 5% of cases, the dural sac is narrowed from birth (congenital malformation). The mechanism involved is usually a decrease in growth of the lumbar canal at the level of the lateral walls, which gives a anteroposterior compression of the dural sac and its content.
Finally, there are some secondary cuts to a fatty deposits inside the lumbar canal. The dural sac and its contents are then compressed and neurological symptoms appear (sensory, motor, sphincter, genital disorders, etc.).
Fatty forms of compression of the dural sac are often observed in patients undergoing long-term treatment with cortisone.
The diagnosis of strictures/compression of the dural sac is based on the clinic (questioning and physical examination) and certain complementary examinations.
The context of weakness and fatigability of the lower limbs with intermittent claudication (lameness and pain when walking with reduced walking distance), sensory neurological signs and genito-sphincter disorders is strongly suggestive of spinal cord compression. Particularly when these signs are aggravated in hyperextension and relieved in delordosis (in a sitting position).
The main differential diagnosis before a intermittent claudication is AOMI (obliterating arteriopathy of the lower limbs). The latter is of vascular origin (clogged artery in the lower limb). It is not accompanied by clinical manifestations such as genito-sphincter disorders, which makes it possible to separate things from the spinal compression.
It is important to specify the compression can sit on all levels of the dural sac (cervical, dorsal, lumbosacral).
The imagery, with the scanner as a reference examination, allows to visualize and evaluate the narrowing/compression of the lumbar canal and the dural sac. It has the disadvantage of exposing the patient to strong radiation.
MRI is an excellent examination to highlight in more detail the different nerve structures affected and the identification of the origin of the compression (herniated disc, etc.). In addition, MRI does not irradiate the patient.
In general, the treatment of this kind of pathologies consists in lift the compression using various methods (most often surgical: cure of a hernia, laminectomy, etc.).
References
[1] H.-K. Ea, F. Lioté, and T. Bardin, “Spinal complications of ankylosing spondyloarthritis”, Journal of Rheumatism Monographs, flight. 82, no 1, p. 42‑47, Feb. 2015, doi: 10.1016/j.monrhu.2015.03.008.
[2] P. Orcel and J. Beaudreuil, “Narrowed lumbar canal: false intermittent claudication”.
[3] “Doctor Debusscher Félix Surgery of the spine and lower limb, narrowing of the spinal canal and clinical repercussions, neurological claudication, description of the various medical and surgical treatments, lumbar recalibration”. http://www.ortho-debusscherfelix.be/cle.html (accessed May 15, 2022).
[4] M. Moukinebillah, S. Khnaba, E. Ouahabi, and M. Jiddane, “Cauda equina syndrome revealing intestinal hernia in the dural sac”, Journal of Neuroradiology, flight. 43, no 2, p. 121, March 2016, doi: 10.1016/j.neurad.2016.01.118.
[5] “Marfan syndrome: definition, symptoms, diagnosis and treatments”, Health on the Net, medical information at the heart of your health. https://www.sante-sur-le-net.com/ Maladies/ Maladies-rares/syndrome-de-marfan/ (consulted on May 12, 2022).
My name is Katia, I am specialized web editor in writing medical articles. Being passionate about medicine and writing, I set myself the goal of making medical information accessible to as many people as possible, through the popularization of even more complex scientific concepts.